You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
Computer-aided design/computer-aided manufacturing (CAD/CAM) technologies have literally revolutionized dental laboratory technology over the past several decades. Concurrently, chairside CAD/CAM systems have become increasingly prevalent, leaving the clinician with a vast array of material and treatment options that were not possible in the past. With regard to minimally invasive dentistry, the availability of a wide range of ceramic materials and recent developments in adhesive technologies have helped make resin-bonded CAD/CAM ceramic restorations extremely popular.1 The long-term clinical success of these restorations depends on various factors, including the physical and optical properties of the ceramic material, tooth preparation design, digital scanning/impression technique, fabrication process, and insertion protocol.1-3 Proper bonding protocols play a crucial role in ensuring optimal adhesion, marginal adaptation, microleakage prevention, and fracture resistance of both the prepared tooth and the restoration.4 Two critical interfaces must always be considered: one to the tooth and the other to the restorative material. While the bonding interface to the tooth is just as important, this article focuses on the resin bond to ceramics, which vary significantly.
Successful ceramic bonds are achieved by establishing a dual bond, involving micromechanical interlocking and true chemical bonding.4 Micromechanical interlocking is achieved through placing priming agents and resin cements onto pretreated micro-retentive bonding surfaces. The composite resin cement should possess physiochemical properties similar to tooth structure, ensuring biocompatibility, resistance to solubility, and chemical and color stability. The actual composition of the resin cement and the pretreatment methods applied to restorative materials and tooth surfaces significantly impact the longevity of bonded ceramic restorations. Surface pretreatment involves steps like acid etching, mechanical roughening, cleaning, and contaminant removal to enhance microscopic surface topography.4
Resin cements typically consist of a bisphenol A-glycidyl methacrylate (bis-GMA) or urethane dimethacrylate resin matrix and 20% to 80% inorganic filler particles.1 They are either light-activated, dual-activated, or auto-activated. Ceramic surface pretreatment methods include etching with hydrofluoric (HF) acid, air-particle abrasion (APA) with aluminum oxide or glass beads, tribochemical silica coating (TBS), and lasers. The choice of treatment depends on the specific ceramic type, composition, and mechanical properties, which in turn determine the restoration's strength and optical characteristics.1
Current CAD/CAM ceramics are classified, based on microstructure, as silica-based ceramics, hybrid ceramics (polymer-infiltrated ceramic network), and oxide ceramics.5 Their clinical applications include inlays, onlays, veneers, resin-bonded prostheses, copings, crowns, and fixed dental prostheses. (Table 1 provides recommended bonding protocols for ceramic restorations.1)
Bonding to Silica-Based Ceramics
Silica-based ceramics are nonmetallic inorganic amorphous materials containing a glass phase. They can be categorized into traditional feldspathic ceramics, leucite-reinforced glass-ceramics, and lithium-silicate ceramics.5 The glass component provides high translucency, excellent esthetic qualities, and a natural appearance. However, their inherent brittleness and relatively low mechanical properties necessitate adhesive bonding for clinical durability.6 The most reliable bond to silica-based ceramics is achieved through a two-step process involving HF acid etching and application of a silane coupling agent.6 Etching time and the concentration varies according to the glass and crystalline content of the specific ceramic.
Bonding to Traditional Feldspathic Ceramics
Feldspathic ceramics consist of a blend of leucite (potassium aluminosilicate) and glass with low to medium flexural strength of up to 120 MPa.1 Their high translucency makes them ideal for various dental applications, including veneering material for metal or ceramic copings, bonded laminate veneers, inlays/onlays, and even full-coverage crowns produced with chairside CAD/CAM technology.5 However, due to their relatively low flexural strength, caution is advised in patients with severe bruxism or in areas of high occlusal loads.6
The bonding process for feldspathic ceramics involves HF acid etching, which selectively dissolves the glass phase, exposing silicon dioxide.7 This dissolution creates topographic changes on the ceramic surface, promoting micromechanical interlocking and chemical bonds with a silane coupling agent and resin cements. HF acid also cleanses and decontaminates bonding surfaces, removing undesirable oxides, phosphates, and other contaminants accrued during manufacturing and try-in procedures. The efficacy of the acid etchant is determined by its concentration and etching time.7 For feldspathic ceramics, 9.8% HF acid applied for 1 to 2 minutes, followed by application of silane, is recommended.4,7 Light-cure composite resin luting agents are suitable for feldspathic veneers as they offer extended working times and simplify the removal of excess cement before light activation. Light-cure composite resins also offer excellent color stability due to the absence of chemical activators like tertiary amines, which can cause long-term color changes.8
Dual-cure resin cements should be used when light penetration is limited.9 They combine the advantages of light- and chemical-activated resin cements, providing adequate polymerization and extended working time. However, some of these resin cements exhibit reduced color stability due to potential oxidation of tertiary amines.8,9 Other bonding protocols, including total-etch, self-etch, and use of self-adhesive resin cements, have demonstrated comparable long-term results.10
Bonding to Leucite-Reinforced Glass-Ceramics
Leucite-reinforced feldspathic ceramics offer higher strength than traditional feldspathic ceramics and are suitable for laminate veneers, anterior crowns, inlays, and onlays.11 These ceramics contain up to 45% leucite by volume, which serves as a reinforcing phase, resulting in medium flexural strength values of up to 140 MPa.1 Leucite-reinforced feldspathic ceramic crowns exhibit high survival rates of 95.2% and offer excellent esthetics after up to 11 years.11 Because of their lower glass phase compared to conventional feldspathic ceramics, the use of 9.8% HF acid etching is recommended for 1 minute.10
Bonding to Lithium-Silicate Ceramics
Lithium-silicate ceramics have gained tremendous popularity due to their esthetic properties and significantly higher flexural strength than all other silica-based ceramics. Restorations are produced through heat pressing or CAD/CAM, containing a glass phase consisting of lithium disilicate and lithium orthophosphate.5 This composition enhances fracture resistance without compromising translucency and offers flexural strength of up to 470 MPa.5 The highly popular IPS e.max® CAD (Ivoclar Vivadent) was recently joined by novel advanced (CEREC Tessera™, Dentsply Sirona) and zirconia-reinforced lithium-silicate ceramics (eg, Celtra Duo, Dentsply Sirona; VITA Suprinity® PC, VITA Zahnfabrik).
Lithium-silicate ceramics are indicated for laminate veneers, inlays/onlays, crowns, three-unit fixed dental prostheses in the anterior region, and implant-supported crowns. Survival rates of 96.7% and 95.2% have been reported for posterior full-coverage crowns and partial-coverage inlays and onlays, respectively, with no instances of debonding during follow-up of 16.9 years.12 Similar to other silica-based ceramics, HF acid etching is recommended to roughen the lithium-silicate surface for effective resin bonding.10 However, due to the removal of the glass phase between the crystals, lithium-silicate ceramics require only 20 seconds of etching with a lower HF acid concentration of 4.6%, followed by the application of a silane coupling agent.10
To simplify bonding protocols and reduce technique sensitivity, manufacturers have introduced universal bonding agents, designed for not only tooth structures but also various dental materials.13 These agents typically contain silanes to broaden their applicability to silica-based ceramics. Nonetheless, for optimal bond strengths, some researchers still recommend applying a separate layer of silane.13
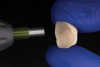
A step-by-step bonding protocol for silica-based ceramics is depicted in Figure 1 through Figure 5.
Bonding to Polymer-Infiltrated Ceramic Network Materials
Polymer-infiltrated ceramic network (PICN) materials, also termed "hybrid ceramics," intend to combine the strength and optical properties of ceramics with the elasticity of polymers.14 These CAD/CAM materials feature interpenetrating networks of ceramic and polymer, with a fine structured leucite enriched with aluminum oxide (86 wt%) into which urethane dimethacrylate (14 wt%) and triethylene glycol dimethacrylate polymers are injected. PICN materials offer reduced brittleness and rigidity, improved flexibility, enhanced fracture toughness, and better machinability compared to traditional silica-based ceramics.5 They require reduced milling times with excellent internal and marginal accuracy. Finishing procedures are significantly simplified, as they do not have to be sintered and only require polishing.5 Moreover, PICN materials exhibit low abrasive wear when opposing teeth come into contact with them.1
Studies on bonding to PICN recommend 9.8% HF acid etching for 1 minute, followed by silanization.14,15 The HF acid etching process exposes the polymer network on the surface as the ceramic matrix is selectively removed.15 The silane chemically bonds with both the ceramics and integrated polymer components, polymerizing with the methacrylate groups found in the resin cements.
A step-by-step bonding protocol for PICN materials is shown in Figure 6 through Figure 11.
It should be noted that resin-matrix ceramics (eg, CERASMART®, GC America Inc.; BRILLIANT Crios, Coltene; Grandio® blocs, Voco) are often erroneously placed in the same material group as PICN. These products have a high ceramic filler content embedded into a polymer matrix.15 They are easy to mill without the need for sintering, and are indicated for many kinds of single-unit restorations. Because their compositions resemble composite resins, resin bonding is typically achieved through APA with aluminum-oxide particles and application of a silane coupling agent.15 To facilitate clinical success, it is advisable to follow manufacturers' instructions for each specific material, which may differ significantly.
Bonding to Zirconia Ceramics
Yttria-stabilized tetragonal zirconium dioxide (Y-TZP) ceramics, also called "zirconia," are nonmetallic polycrystalline ceramic materials with high fracture strength and toughness and at least some degree of translucency.5 They have widely replaced porcelain-fused-to-metal restorations.5,16-18 The lack of a glass phase affects the efficacy of HF acid etching, necessitating alternative surface pretreatment methods when resin bonding is applied.
Y-TZP restorations are fabricated with CAD/CAM technologies; initially this was done for copings and frameworks to be veneered with layering porcelain, while more recently it encompasses full-contour monolithic restorations, ranging from partial-coverage tooth-supported to full-mouth implant-supported reconstructions.16-18 The mechanical and optical properties of Y-TZP are largely determined by its yttria content. First on the market was 3Y-TZP, which is also considered "conventional zirconia." High-translucent 4Y-TZP and 5Y-TZP are newer generations of zirconia with enhanced esthetics.19 The increased yttria content leads to a higher percentage of cubic-phase particles, making them more translucent than 3Y-TZP. However, their decreased flexural strength limits their clinical indications to single units and short-span fixed dental prostheses.19
The various zirconia types are offered in large discs for milling and fabrication in the dental laboratory (eg, Katana™ HTML, STML, and UTML, Kuraray Noritake Dental; IPS e.max® ZirCAD, Ivoclar Vivadent). High-translucent zirconia blocks are also offered for chairside CAD/CAM systems, such as CEREC® Zirconia (Dentsply Sirona), Katana™ Zirconia One (Kuraray Noritake Dental), VITA YZ (VITA Zahnfabrik), Lava™ Zirconia Block (3M Oral Care), and IPS e.max® ZirCAD (Ivoclar Vivadent). With a special chairside furnace and speed sintering program, the sintering of a single crown can take less than 19 minutes.5 Multi-chromatic zirconia blocks with varying chroma levels from dentin to enamel layers have become standard. The latest developments, however, include multi-translucent blocks (eg, Katana™ YML, Kuraray Noritake Dental; IPS e.max® ZirCAD Prime Esthetic, Ivoclar Vivadent) with layers of different translucency levels for increased esthetics of monolithic zirconia restorations.
All of these zirconia formulations offer sufficient flexural strength such that they do not require resin bonding for definitive insertion of full-coverage restorations; they can be conventionally cemented as long as restoration retention and fit meet the necessary criteria.2,5,16 If such criteria are not met, or when resin-bonded restorations such as partial-coverage restorations or resin-bonded fixed dental protheses are fabricated, proper bonding protocols become essential. These differ substantially between silica-based and oxide-based ceramics.4 Several surface pretreatment methods improve resin bonds to 3Y-TZP, including APA, TBS, low-fusion porcelain application, hot chemical etching solutions, selective infiltration etching, laser irradiation, plasma spraying, and zirconia ceramic powder coating.2 In vitro studies and systematic reviews concur that a combination of mechanical and chemical pretreatment is necessary for long-term durable resin bonds to 3Y-TZP.2 Applying 10-methacryloyloxydecyl dihydrogen phosphate (MDP) monomer or other phosphate ester monomer-based primers and resin cements on surface-treated 3Y-TZP has been found to provide superior and long-term durable resin bonds. These functional monomers chemically bond to oxides in Y-TZP.2,4,19,20
This preferred bonding protocol is summarized in the "APC" zirconia bonding concept, consisting of three key steps: APA with alumina or silica-coated alumina particles (step "A"), priming of the air-abraded surfaces with an MDP or other phosphate-monomer-based primer (step "P"), and use of a dual- or self-cure composite resin cement (step "C").20 APA with small alumina or silica-coated alumina particles (50 µm to 60 µm) at low pressure (2 bar) is sufficient. Earlier concerns about the possibly damaging effects of APA on Y-TZP have been shown to be unfounded.21 This is true even when bonding to high-translucent zirconia, as a recent systematic review found no negative effect of APA on the flexural strength of these restorations.19 Various surface pretreatment methods have been explored, including APA with alumina or glass beads, TBS, plasma treatment, piranha etching, and hot chemical etching solutions. The preferred bonding protocol is the same as for 3Y-TZP zirconia: APC.19
A step-by-step bonding protocol for Y-TZP is depicted in Figure 12 through Figure 17.
Ceramic Cleaning
To clean ceramic surfaces after intraoral restoration try-in, alcohol solutions such as ethanol and isopropanol, as well as phosphoric acid, can be effective. Silica-based ceramics benefit from 5-minute ultrasonic cleaning before the application of silane coupling agents. However, for zirconia and other metal-oxide ceramics, APA with alumina particles has been found to be the most effective decontamination and cleaning method.22 It is important to note that recontamination can occur even when the restoration is only exposed to air, leading to lower bond strength values with zirconia when there is a longer time gap between APA and primer application.23 The primer ideally should be applied immediately after APA. When clinicians do not have access to a sandblasting unit or microetcher, they may have the dental laboratory perform APA on their bonded zirconia restorations. Cleaning agents (eg, Ivoclean, Ivoclar Vivadent; Katana™ Cleaner, Kuraray Noritake Dental; ZirClean®, BISCO) are effective in removing contaminants and proteins from bonding surfaces of ceramics and other restorative materials following intraoral try-in.22
Some recent "ceramic primers" include both silane and special phosphate monomers like MDP, making them suitable and effective for both silica-based and Y-TZP ceramics.
Proper Isolation
For all types of intraoral adhesive bonding procedures, proper isolation of the operating field is critically important to prevent contamination, which jeopardizes clinical success. Rubber dam, gauze pieces, cotton rolls, Teflon tape, gingival retraction cords, and/or appropriate suction devices are needed to limit contamination from moisture, bacteria, saliva, and blood, ultimately improving the quality and longevity of bonded ceramic restorations. A recent clinical in situ study by Falacho et al indicated that in the oral cavity, even moisture from exhaling significantly reduces bond strength to enamel and concluded that rubber dam isolation should be mandatory.24
Conclusion
The longevity of resin-bonded ceramic restorations hinges on the strength and durability of the resin-ceramic bonding interface. The choice of bonding protocol is determined by the type and composition of the ceramic material used. Typically, this protocol involves surface pretreatment and application of a priming agent to establish strong and long-lasting resin bonds.
About the Authors
Markus B. Blatz, DMD, PhD
Professor of Restorative Dentistry, Chair, Department of Preventive and Restorative Sciences, and Assistant Dean, Digital Innovation and Professional Development, University of Pennsylvania School of Dental Medicine, Philadelphia, Pennsylvania
Amirah Alammar, BDS, certified in prosthodontics, Doctorate
Private Practice, Sijam Medical Center, Riyadh, Saudi Arabia
Jose M. Ayub, DDS
Visiting Scholar, Department of Preventive and Restorative Sciences, University of Pennsylvania School of Dental Medicine, Philadelphia, Pennsylvania
Francisco Rojas, DDS
Visiting Scholar, Department of Preventive and Restorative Sciences, University of Pennsylvania School of Dental Medicine, Philadelphia, Pennsylvania
Julian Conejo, DDS, MSc
Assistant Professor, Clinical Restorative Dentistry, and Director, Chairside CAD/CAM Dentistry, Department of Preventive and Restorative Sciences, University of Pennsylvania School of Dental Medicine, Philadelphia, Pennsylvania
Queries to the author regarding this course may be submitted to authorqueries@broadcastmed.com.
References
1. Blatz MB, Conejo J, Alammar A, Ayub J. Current protocols for resin-bonded dental ceramics. Dent Clin North Am. 2022;66(4):603-625.
2. Blatz M, Vonderheide M, Conejo J. The effect of resin bonding on long-term success of high-strength ceramics. J Dent Res. 2018;97(2):132-139.
3. Morimoto S, Rebello de Sampaio FB, Braga MM, et al. Survival rate of resin and ceramic inlays, onlays, and overlays: a systematic review and meta-analysis. J Dent Res. 2016;95(9):985-994.
4. Blatz MB, Sadan A, Kern M. Resin-ceramic bonding: a review of the literature. J Prosthet Dent. 2003;89(3):268-274.
5. Blatz MB, Conejo J. The current state of chairside digital dentistry and materials. Dent Clin North Am. 2019;63(2):175-197.
6. Beier US, Dumfahrt H. Longevity of silicate ceramic restorations. Quintessence Int. 2014;45(8):637-644.
7. Venturini AB, Prochnow C, Rambo D, et al. Effect of hydrofluoric acid concentration on resin adhesion to a feldspathic ceramic. J Adhes Dent. 2015;17(4):313-320.
8. Kowalska A, Sokolowski J, Bociong K. The photoinitiators used in resin based dental composite-a review and future perspectives. Polymers (Basel). 2021;13(3):470.
9. Faria-E-Silva AL, Pfeifer CS. Development of dual-cured resin cements with long working time, high conversion in absence of light and reduced polymerization stress. Dent Mater. 2020;36(10):e293-e301.
10. Farias DCS, Gonçalves LM, Walter R, et al. Bond strengths of various resin cements to different ceramics. Braz Oral Res. 2019;33:e095.
11. Fradeani M, Redemagni M. An 11-year clinical evaluation of leucite-reinforced glass-ceramic crowns: a retrospective study. Quintessence Int. 2002;33(7):503-510.
12. Malament KA, Margvelashvili-Malament M, Natto ZS, et al. Comparison of 16.9-year survival of pressed acid etched e.max lithium disilicate glass-ceramic complete and partial coverage restorations in posterior teeth: performance and outcomes as a function of tooth position, age, sex, and thickness of ceramic material. J Prosthet Dent. 2020;126(4):533-545.
13. Nagarkar S, Theis-Mahon N, Perdigão J. Universal dental adhesives: current status, laboratory testing, and clinical performance. J Biomed Mater Res Part B Appl Biomater. 2019;107(6):2121-2131.
14. Conejo J, Ozer F, Mante F, et al. Effect of surface treatment and cleaning on the bond strength to polymer-infiltrated ceramic network CAD-CAM material. J Prosthet Dent. 2021;126(5):698-702.
15. Spitznagel FA, Horvath SD, Guess PC, Blatz MB. Resin bond to indirect composite and new ceramic/polymer materials: a review of the literature. J Esthet Restor Dent. 2014;26(6):382-393.
16. Ozer F, Mante FK, Chiche G, et al. A retrospective survey on long-term survival of posterior zirconia and porcelain-fused-to-metal crowns in private practice. Quintessence Int. 2014;45(1):31-38.
17. Blatz MB, Hariton-Gross K, Anadioti E, et al. Prospective 5-year clinical evaluation of posterior zirconia fixed dental prostheses veneered with milled lithium disilicate (CADon). J Esthet Restor Dent. 2022; 34(1):136-144.
18. Luna-Domínguez CR, Luna-Domínguez JH, Blatz M. Full-mouth rehabilitation in a completely digital workflow using partially adhesive monolithic zirconia restorations. J Esthet Restor Dent. 2023. doi: 10.1111/jerd.13048.
19. Alammar A, Blatz MB. The resin bond to high-translucent zirconia - a systematic review. J Esthet Restor Dent. 2022;34(1):117-135.
20. Blatz MB, Alvarez M, Sawyer K, Brindis M. How to bond zirconia: the APC concept. Compend Contin Educ Dent. 2016;37(9):611-617.
21. Ozer F, Naden A, Turp V, et al. Effect of thickness and surface modifications on flexural strength of monolithic zirconia. J Prosthet Dent. 2018;119(6):987-993.
22. Wattanasirmkit K, Charasseangpaisarn T. Effect of different cleansing agents and adhesive resins on bond strength of contaminated zirconia. J Prosthodont Res. 2019;63(3):271-276.
23. Al-Akhali M, Al-Dobaei E, Wille S, et al. Influence of elapsed time between airborne-particle abrasion and bonding to zirconia bond strength. Dent Mater. 2021;37(3):516-522.
24. Falacho RI, Melo EA, Marques JA, et al. Clinical in-situ evaluation of the effect of rubber dam isolation on bond strength to enamel. J Esthet Restor Dent. 2023;35(1):48-55.