You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
The delivery of orthodontic treatment in skeletally mature adolescents and young adults has increased in recent years. Both groups of patients lack the adaptative craniofacial growth that children have.1 It has been proposed that proper arch coordination in maxillary and mandibular skeletal transverse dimensions is paramount before vertical and sagittal corrections are attempted.2,3 There are several general factors for clinicians to consider when dealing with complex maxillary transverse deficiencies.
Commonly in maxillary transverse deficiencies, the mandibular posterior teeth are lingually tipped, giving a false clinical impression of good buccolingual coordination between the maxillary and mandibular arches. In other instances, the patient presents a posterior crossbite.2,3 For decades, the posteroanterior cephalometric x-ray has been used to assess maxillary transverse dimensions compared to the mandibular ones based on the patient's chronological age.4 More recently, cone-beam computed tomography (CBCT) imaging has been recommended to determine craniofacial transverse skeletal imbalances.5 A general rule suggests that there should be 5 mm more width transversally in the maxilla than in the mandible at the level of the permanent first molars.5
In skeletally mature patients with a transverse skeletal discrepancy larger than 5 mm, a temporary anchorage device (TAD)-assisted6 or surgically assisted palatal expansion is indicated.3 In transverse corrections, the overall treatment goal is to obtain skeletal apical base improvements that are as parallel as possible in both the anterior and posterior regions of the maxilla. Achieving the same amount of expansion in the anterior and posterior regions is the main objective concerning the midpalatal suture opening.6 Dental compensation tipping must be avoided, as it will likely lead to periodontal problems (ie, fenestrations and dehiscences) and unstable results in the long term.7 When an exclusively toothborne expansion is used, dental tipping will be observed.8 In this sense, when dental structures are not used to support the expander, there is no need to overexpand with either TAD-assisted6 or surgically assisted TAD-supported palatal expansion.2,3
Occlusal interferences due to a narrow maxilla can lead to an increased curve of Wilson and should be corrected.2,3,6,8 They tend to produce a discrepancy between centric relation and centric occlusion with functional implications.3
Determining Midpalatal Suture Skeletal Maturation
Angilieri et al were the first authors to describe a midpalatal suture maturation classification to simplify palatal expansion decision-making.9 A thorough understanding of the degree of interdigitation can aid clinicians in determining which patients are better candidates for TAD-assisted rapid palatal expansion and which ones are more suited for surgically assisted rapid palatal expansion. Surgery should be avoided if it is unnecessary.6
In late adolescents and young adults, transverse maxillary constrictions can be treated nonsurgically with the support of palatal TADs. Surgical approaches are more often indicated at later stages.9 Kwak et al showed that more adults presented non-fused midpalatal sutures than previously thought.10 Jimenez-Valdivia et al reported consistent midpalatal suture opening in patients 20 years and older when CBCT reconstructions predicted that nonsurgical expansion was possible.11 Some clinicians consider other diagnostic parameters for skeletal maturity, such as vertebrae maturation and hand-wrist skeletal maturation, among others.12,13
Palatal Constriction Management
It is known that the midpalatal suture is not the primary source of resistance to palatal expansion, but rather the circummaxillary sutures, pterygoid plates, and malar bones are. Still, there is not as much "bridging" from one palatal half to the other in early developmental stages, and this facilitates an easier palatal expansion.14
Mommaerts used a thick transpalatal screw anchored directly to the palate for expansion in adults.15 His rationale was to avoid dental anchorage to eliminate tipping side effects such as dentoalveolar inclinations and potential periodontal complications. Lee et al incorporated palatal TADs to produce nonsurgical expansion in young adults.16 Their idea was to avoid the surgical cuts necessary in surgically assisted rapid palatal expansion. Ludwig et al described how the amount of bone around palatal TADs was the most critical factor for success.17 They compared cortical palatal bone with interradicular bone in the buccal segments and determined that the palatal bone cortex was of higher quality.
The use of CBCTs to guide the placement of palatal TADs has also been described. Maino et al proposed positioning guides by using a thermoplastic template constructed on the patient's model to guide palatal TAD placement.18 They suggested that using CBCTs in these cases should provide precision for placing TADs.
Different systems have been proposed for TAD-supported palatal expansion, including hybrid systems6,19,20 or those supported solely by TADs placed on the palate.16 Hybrid expanders incorporate the use of bands on teeth (usually maxillary first molars) combined with the TAD placed in the palate.6,19,20 Moon et al compared a lateral palate wall expansion system with a hybrid expander.20 The authors concluded that lateral palate wall expanders produced more alveolar bone inclination; more buccal inclination of the anchored teeth (permanent first molars) was observed in the hybrid systems. They also described the height and width of the alveolar bone on the buccal surface of the maxillary permanent first molar patients. They determined less bone was present in the hybrid group than in the purely bone-supported group. Finally, they also reported more dehiscences on the hybrid group but not more fenestrations.
Digital flow models have been reported as a means to increase predictability in both hybrid expansion systems and bone-anchored systems.18,19,21 Cantarella et al described integrating STL files (dental scans) with CBCTs. The quality of bone, more so than the quantity of bone, was assessed during their planning.19 Lo Giudice et al analyzed digital flow through 3D maxillary superimpositions.21 They reported that palatal TADs were placed in the best angulation and position through tailored virtual guides.
In summary, lateral palate wall expanders may be a practical approach to obtain nonsurgical expansion in skeletally mature adolescents and young adults.22 They are bandless, so the use of teeth as anchors is avoided. Thus, no force is exerted on teeth, preventing side effects that can result from toothborne expanders, such as extrusion of anchor molars, premature contact of hanging palatal cusps produced by tooth-supported methods, and exertion of buccal forces on teeth that may lead to periodontal problems.16,22
Placement and Activation of Virtually Guided Lateral Palate Wall Expander
The protocol for placing and activating a virtually guided lateral palate wall expander begins with a digital scan of the patient's mouth. Using the acquired information, a virtual guide is constructed with software and subsequently printed. This guide allows for the placement of TADs in the areas where bone availability is optimal.18,19,21
On a second visit, the guide is used, and the expander is inserted. The patient first receives infiltrative anesthesia with lidocaine 2%. The guide is then utilized to place four TADs, typically 10 mm to 12 mm long and 1.8 mm to 2 mm wide. This length considers the 4 mm or 5 mm width of the palatal bone and palatal mucosa. Allowing at least 5 mm of the TAD in the palatal bone as anchorage is desirable.
Usually, palatal TAD placement is mesial to the maxillary first molar and between the premolars. However, the TAD location can be moved forward or backward to obtain the optimum bone density. Placement is done with a slow-speed handpiece. The convergence between the roots of the premolars is not a problem because the TAD is virtually guided. Another advantage of this approach is if tooth germs of unerupted cuspids are present, they can be avoided. Sometimes the surgical guide can be cut in half to obtain better lateral wall placement. Depending on bone availability, in some instances angulating the TADs allows bicortical engagement. It is also important to leave 4 mm or 5 mm of space between the border of the appliance and the gingiva on the palatal side. After the miniscrews, ie, TADs, are satisfactorily placed, the acrylic expander is incorporated through the use of either resin cement placed through four holes in the acrylic component or acrylic soft-tissue conditioning material. If the latter material is used rather than four holes in the appliance, undercuts are made on the acrylic where the four TADs are located.
After proper cementation, the appliance is activated by four turns (0.25 mm each) of the jackscrew. Usually, an ultra-flat 12 mm jackscrew may be used. After this initial activation, subsequent activation consists of two daily turns until the desired expansion is achieved. As explained earlier, the final amount of expansion is determined based on the initial CBCT by subtracting the maxillary width from the mandibular width and adding 5 mm.
In some instances more than one expander may be required in very deficient upper jaws in the transverse dimension. In such a case, the expander is removed, and a new one is placed using the four TADs already installed in the palate. Other times, in older patients, an extra TAD may be added per side (making it a six-TAD appliance). Finally, if anterior traction of the maxilla is required, extension arms can be incorporated into the appliance.
The patient must be advised on the importance of maintaining good oral hygiene with the appliance. Irrigators are helpful in this regard. Should food particles get trapped under the appliance, they can produce an undesirable odor. During orthodontic control appointments, professional cleaning might be done to clean the area thoroughly.
After the expansion, the jackscrew hole is sealed, and the appliance is left in place for 6 months to allow bone formation in the generated space in the midpalatal suture. The upper midline diastema formed through expansion is closed through fixed orthodontic appliances (brackets), and orthodontics is continued. Inflammation should not pose a problem once the appliance is removed. Tissue fully heals typically in 4 or 5 days.22
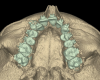
This treatment process is demonstrated in the case presented in Figure 1 through Figure 17. A 15-year-old female patient had a severe posterior bilateral crossbite associated with a very narrow maxilla, severe crowding in the narrow maxillary arch, and mesially inclined posterior teeth in the mandibular arch. The transverse deficiency of the maxilla was diagnosed clinically, photographically, and through CBCT measurements. Treatment consisted of using a miniscrew-supported virtually guided lateral wall expander to widen the maxilla and buccal shelf miniscrews in the lower posterior segments to upright the mesially tipped lower buccal segments. The treatment was combined with the use of 0.22 straight wire appliances with a Roth prescription for 24 months in both arches. The dentofacial and dental results and post-expansion CBCT images demonstrated the correction of the transverse discrepancy as the basis for the full correction of the case. Well-aligned arches in a good class I occlusion and a full, broad smile without negative space in the buccal corridors complemented the treatment result. As seen in this case, documentation of the changes noted on the CBCTs throughout the treatment is crucial in assessing the effects produced with this modality.
Assisting Palatal Expansion in Skeletally Mature Patients
With other TAD-supported systems,6,19,20 corticopunctures administered under infiltrative anesthesia have been proposed as a means for debilitating midpalate sutures through microperforations with a TAD or small round bur.23 Some clinicians have used virtual guides to produce them to improve microperforation placement. Critics of this technique argue that, as mentioned earlier, the midpalatal suture is not the primary resistance source to palatal expansion, but rather the malar bone, pterygoid plates, and circummaxillary sutures are the main sources of resistance. Furthermore, only very few case reports demonstrating this approach are available.
Surgically Assisted Palatal Expansion With Virtually Guided Lateral Wall Expander
With TAD-supported expansion, it is possible that the midpalatal sutural split may not be able to be accomplished. This is especially so in men older than 25 years due to increased skeletal resistance.9 Even with the use of paramedial suture expanders, surgery might be necessary.6,19,20 In such cases, a surgically assisted rapid palatal expansion protocol can be used to incorporate a lateral wall expander.
Initially, Betts and Ziccardi described a bilateral maxillary osteotomy from the piriform aperture to the pterygomaxillary fissure and midpalatal suture separation from the anterior nasal spine to the posterior nasal spine. The osteotomy was performed parallel to the occlusal plane with a step in the maxillary buttress to avoid interfering with the expansion.24 Surgical cuts were proposed 5 mm above apices, and liberation of the nasal septum and pterygoid plates was performed.25
Hernandez Alfaro et al proposed using minimally invasive corticotomies to liberate the mechanical osseous impediment to palatal expansion.26 This procedure is done under general or local anesthesia and endovenous sedation.27,28 A 10-mm-thick flap below the mucogingival line is performed to control hemostasia with either a #15 blade or an electric scalpel. The surgical approach is limited to the maxillary lateral incisors with 2 cm to 3 cm lengths to reduce morbidity and recovery time.26 After this, a subperiosteal dissection from the piriform aperture to the pterygomaxillary suture is completed. Minimally invasive protocols describe a subspinal osteotomy.29 Next, a subspinal osteotomy is performed to maintain the ligaments attached to the anterior nasal spine and facilitate dissection from the nasal floor. Then the cartilaginous nasal septum is separated from the bone to avoid a septal deviation during maxillary expansion. The jackscrew is activated 2 mm at surgery (eight turns of 0.025 mm each) to create further tension to separate the palatal halves.
Using a 30 mm reciprocating blade, a horizontal osteotomy is completed on the buccal surface of the maxilla at least 5 mm above the apex of the canine, extending from the pyramid aperture to the maxillary tuberosity. This is done to debilitate the nasomaxillary and zygomatic-maxillary buttress. Osteotomy allows evident liberation of the area to prevent osseous interferences during expansion. A vertical midline osteotomy can be performed by inserting a piezotome anteroposteriorly with a 10 mm reciprocating blade or chisel to generate the split between the two maxillary central incisors. After this, a thicker chisel is inserted to perform soft rotatory movements to complete the fracture line vertically to the base of the papillae of the maxillary central incisors. An anteroposterior movement is performed through the posterior nasal spine. The expander can be activated for a couple of turns to observe if a symmetric split has been achieved. Wound closure with a 4-0 vicryl suture is performed. It is crucial to avoid widening the base of the nose by performing the V-Y closure technique.
Final Considerations
Virtual guidance allows TAD placement in optimal bone (in quantity and quality) as determined by a CBCT. Such guides also enable the avoidance of contact with the roots of premolars in the area where there is root convergence. The TAD-supported acrylic lateral wall expander is a simple yet effective mechanism for managing transverse discrepancies in late adolescents and young adults. A further advantage is that it can be incorporated into surgically assisted rapid palatal expansion protocols if the initial nonsurgical approach fails to deliver the maxillary sutural split.
Other TAD-supported expander systems are also available. Some use the anterior portion of the maxillae for TAD placement,30 while others use paramedial suture-placed TADs.6,19,20,31 The approach described in this article is but one tool in the orthodontist's armamentarium when treating maxillary transverse deficiencies.
About the Authors
Miguel Hirschhaut, DDS, PhD
Private Practice limited to Orthodontics, Caracas, Venezuela
Nelson Leon, DDS
Private Practice limited to Oral and Maxillofacial Surgery, Caracas, Venezuela
Asdrubal Pereira, DDS
Private Practice limited to Oral and Maxillofacial Surgery, Caracas, Venezuela
Carlos Flores-Mir, DDS, DSc
Professor, Division of Orthodontics, Department of Dentistry, University of Alberta, Edmonton, Alberta, Canada; Part-time Private Practice limited to Orthodontics, Edmonton, Alberta, Canada
Queries to the author regarding this course may be submitted to authorqueries@broadcastmed.com.
References
1. Kokich VG. Esthetics: the orthodontic-periodontic restorative connection. Semin Orthod. 1996;2(1):21-30.
2. Betts NJ, Vanarsdall RL, Barber HD, et al. Diagnosis and treatment of transverse maxillary deficiency. Int J Adult Orthodon Orthognath Surg. 1995;10(2):75-96.
3. Vanarsdall RL Jr. Transverse dimension and long-term stability. Semin Orthod. 1999;5(3):171-180.
4. Ricketts RM. Introducing Computerized Cephalometrics. Denver, CO: Rocky Mountain Data Systems; 1969.
5. Tamburrino RK, Boucher NS, Vanarsdall RL, Secchi A. The transverse dimension: diagnosis and relevance to functional occlusion. RWISO Journal. September 2010:13-21.
6. Brunetto DP, Sant'Anna EF, Machado AW, Moon W. Non-surgical treatment of transverse deficiency in adults using microimplant-assisted rapid palatal expansion (MARPE). Dental Press J Orthod. 2017;22
(1):110-125.
7. Vanarsdall R, Secchi A. Periodontal-orthodontic interrelationships. In: Graber L, Vanarsdall R, Vig W, eds. Orthodontics: Current Principles and Techniques. 5th ed. Philadelphia, PA: Elsevier Mosby; 2011:807-841.
8. Baccetti T, Franchi L, Cameron CG, McNamara JA Jr. Treatment timing for rapid maxillary expansion. Angle Orthod. 2001;71(5):343-350.
9. Angelieri F, Cevidanes L, Franchi L, et al. Midpalate suture maturation: classification method for individual assessment before rapid maxillary expansion. Am J Orthod Dentofacial Orthop. 2013;144(5):759-769.
10. Kwak KH, Kim SS, Kim YI, Kim YD. Quantitative evaluation of midpalatal suture maturation via fractal analysis. Korean J Orthod. 2016;46(5):323-330.
11. Jimenez-Valdivia LM, Malpartida-Carrillo V, Rodríguez-Cárdenas YA, et al. Midpalatal suture maturation stage assessment in adolescents and young adults using cone-beam computed tomography. Prog Orthod. 2019;20(1):38.
12. Baccetti T, Franchi L, McNamara JA Jr. An improved version of the cervical vertebral maturation (CVM) method for the assessment of mandibular growth. Angle Orthod. 2002;72(4):316-323.
13. Isfeld D, Lagravere M, Leon-Salazar V, Flores-Mir C. Novel methodologies and technologies to assess mid-palatal suture maturation: a systematic review. Head Face Med. 2017;13(1):13.
14. Babacan H, Sokucu O, Doruk C, Ay S. Rapid maxillary expansion and surgically assisted rapid maxillary expansion effects on nasal volume. Angle Orthod. 2006;76(1):66-71.
15. Mommaerts MY. Transpalatal distraction as a method of maxillary expansion. Br J Oral Maxillofac Surg. 1999;37(4):268-272.
16. Lee KJ, Park YC, Park JY, Hwang WS. Miniscrew-assisted non-surgical palatal expansion before orthognathic surgery for a patient with severe mandibular prognathism. Am J Orthod Dentofacial Orthop. 2010;137(6):830-839.
17. Ludwig B, Glasl B, Bowman SJ, et al. Anatomical guidelines for miniscrew insertion: palatal sites. J Clin Orthod. 2011;45(8):433-441.
18. Maino BG, Paoletto E, Lombardo L 3rd, Siciliani G. A three-dimensional digital insertion guide for palatal miniscrew placement. J Clin Orthod. 2016;50(1):12-22.
19. Cantarella D, Savio G, Grigolato L, et al. A new methodology for the digital planning of micro-implant-supported maxillary skeletal expansion. Med Devices (Auckl). 2020;13:93-106.
20. Moon HW, Kim MJ, Ahn HW, et al. Molar inclination and surrounding alveolar bone change relative to the design of bone-borne maxillary expanders: a CBCT study. Angle Orthod. 2020;90(1):13-22.
21. Lo Giudice A, Quinzi V, Ronsivalle V, et al. Description of a digital work-flow for CBCT-guided construction of micro-implant supported maxillary skeletal expander. Materials (Basel). 2020;13(8):1815.
22. Vanarsdall R, Blasi I, Evans M, Kocian P. Rapid maxillary expansion with skeletal anchorage vs. bonded tooth/tissue borne appliances. J Clin Rev RMO. 2012;19-22.
23. Suzuki SS, Braga LFS, Fujii DN, et al. Corticopuncture facilitated microimplant-assisted rapid palatal expansion. Case Rep Dent. 2018;2018:1392895.
24. Betts NJ, Ziccardi VB. Surgically assisted maxillary expansion. In: Fonseca RJ, ed. Oral and Maxillofacial Surgery. Philadelphia, PA: W.B. Saunders; 2000:211-231.
25. Pogrel MA, Kaban LB, Vangervik K, Baumrind S. Surgically assisted rapid maxillary expansion in adults. Int J Adult Orthodon Orthognath Surg. 1992;7(1):37-41.
26. Hernandez-Alfaro F, Mareque Bueno J, Diaz A, Pages CM. Minimally invasive surgically assisted rapid palatal expansion with limited approach under sedation: a report of 283 consecutive cases. J Oral Maxillofac Surg. 2010;68(9):2154-2158.
27. Bays RA, Greco JM. Surgically assisted rapid palatal expansion: an outpatient technique with long-term stability. J Oral Maxillofac Surg. 1992;50(2):110-115.
28. Dann JJ. Outpatient oral and maxillofacial surgery: transition to a surgicenter setting and outcome of the first 200 cases. J Oral Maxillofac Surg. 1998;56(5):572-577.
29. Mommaerts MY, Abeloos JV, De Clercq CA, Neyt LF. The effect of the subspinal Le Fort I-type osteotomy on interalar rim width. Int J Adult Orthodon Orthognath Surg. 1997;12(2):95-100.
30. Wilmes B, Tarraf N, Drescher D. Treatment of maxillary transversal deficiency by using a mini-implant-borne rapid maxillary expander and aligners in combination. Am J Orthod Dentofacial Orthop. 2021;160(1):147-154.
31. Brunetto DP, Moschik CE, Dominguez-Mompell R, et al. Mini-implant assisted rapid palatal expansion (MARPE) effects on adult obstructive sleep apnea (OSA) and quality of life: a multi-center prospective controlled trial. Prog Orthod. 2022;23(1):3.