You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
According to the American College of Prosthodontists, more than 36 million Americans do not have any teeth, and 120 million more are missing at least one tooth.1 Edentulism affects the most vulnerable populations, which are the elderly and those who are economically disadvantaged. In the geriatric population, the ratio of edentulous individuals is 2 to 1; about 23 million elderly people in the United States are completely edentulous, and about 12 million are edentulous in one arch. Ninety percent of those who have edentulism have dentures, and about 15% of the edentulous population has dentures made each year.
Statistics also indicate that the number of edentulous patients will grow significantly in the next two decades. The consequences of edentulism may include significant nutritional changes, obesity, diabetes, coronary artery disease, and some forms of cancer, making edentulism a negative factor in a person's well-being if not treated effectively.
Digital technologies in dentistry continue to grow in usage and become more accessible to dental professionals worldwide. Proper understanding of their indication and application with appropriate clinical-laboratory protocols is vital for their successful implementation. This article describes new workflows for complete dentures, immediate dentures, overdentures, and fixed full-arch restorations with the implementation of intraoral scanners and photogrammetry.
Complete Dentures
Traditional protocols for the fabrication of complete dentures require numerous time-consuming appointments, which can contribute to making the patient experience unpleasant when either new dentures need to be fabricated or existing dentures replaced.2 Most of the computer-aided design/computer-aided manufacturing (CAD/CAM) systems for dental laboratory use have the ability to design and produce complete dentures via scanning of the master casts once they are mounted on a semi-adjustable articulator. This workflow combines analog and digital steps. One of its main advantages is that creating a duplicate of a previous prosthesis is straightforward because the information is saved in the software. The clinical steps, however, still require the same number of appointments as strictly analog protocols.3
When digital impressions are made using an intraoral scanner (IOS), specific tools are recommended for determining incisal edge position (eg, a papillameter) and centric relation (eg, a prefabricated tray for individual bite registration) to allow scanning for maxillo-mandibular correlation.
CAD/CAM complete dentures can be fabricated using several different methods4:
The denture base can be milled from a pink polymethyl methacrylate (PMMA) disc, and splinted teeth milled from another PMMA disc with the required tooth color. A specific bonding system and air-particle abrasion are used to bond these two elements together.
A monolithic denture can be milled from a pink/white PMMA disc, requiring a specific software and milling strategy to accommodate the denture in its correct 3-dimensional (3D) spatial position.
The base can be milled or 3D printed with prefabricated denture teeth that can be selected in the software from a library provided by the manufacturer, based on the desired size and shape of the teeth. A specific bonding system and air-particle abrasion are used to bond the teeth to the base.
With these three options, surface characterization is possible with indirect composite materials. As the development of 3D printing resins has continued to expand, specific resins are now available to 3D print monolithic dentures that also can be characterized with indirect composites to simulate pink gingival areas.5
Clinical Case: Complete Dentures
An edentulous female patient with defective pre-existing complete dentures presented for consultation (Figure 1). Clinical evaluation revealed moderate ridge absorption. After preliminary impressions for custom tray fabrication were made, final impressions were made with polyvinyl siloxane. Master casts and wax rims were made following established guidelines. Vertical dimension of occlusion was established and intermaxillary records in centric relation were used to mount the casts on a semi-adjustable articulator.6
A high-resolution laboratory scanner was used to scan the maxillary and mandibular casts and wax rims for virtual articulation. The complete dentures were designed with a laboratory CAD/CAM software (Figure 2).
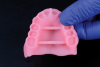
Denture bases were milled from PMMA pink acrylic discs in a five-axis milling machine. The digital libraries of prefabricated acrylic denture teeth have been optimized with a "no-grind design" that virtually eliminates intaglio breakthrough (Figure 3). Individual teeth were bonded to the milled bases after air-particle abrasion with 50-micron aluminum-oxide particles.
After try-in and delivery, a follow-up appointment was scheduled. The patient expressed contentment regarding the functional and esthetic outcome of the new dentures (Figure 4).
Immediate Dentures
Making conventional impressions on teeth with high mobility and retentive areas due to loss of soft tissue presents a challenge to clinicians.7 With the constant development of intraoral scanners, full-arch digital impressions now seem to be a viable alternative to conventional methods. Creating a contactless impression on resilient tissues is advantageous for the internal adaptation of tissue-supported prostheses by applying a truly mucostatic impression approach.8 Linear movements when scanning, lip and cheek retraction, and humidity control are important factors to achieve an accurate intraoral impression.9
Clinical Case: Partial Dentures
A partially edentulous female patient with failing fixed dental prostheses on highly mobile abutment teeth presented for implant consultation (Figure 5). Full-arch maxillary, mandibular, and buccal scans were made with an IOS with the use of a lip retractor to facilitate imaging of soft tissues (Figure 6). The use of a jig for a more stable intermaxillary registration for highly mobile teeth was indicated.
Maxillary teeth were virtually extracted in the CAD software, and an immediate denture was designed with prefabricated acrylic denture teeth from a digital library. The denture base was 3D printed with a pink denture resin material (Figure 7). Use of a methyl methacrylate-based self-curing two-component bonding system enabled fixation of the teeth to the 3D-printed base (Figure 8).
After extraction of all maxillary teeth and removal of the abutment on a pre-existing implant, the immediate denture was delivered (Figure 9). Follow-up appointments and dietary recommendations were given to the patient.
In clinical situations where severe resorption after teeth extraction is present, the 3D-printed denture can be relined with conventional reline materials.10
Overdentures
For edentulous patients with severe bony ridge resorption, two non-splinted implants for mandibular overdentures and four non-splinted implants for maxillary overdentures with a metal framework can be used to provide superior retention.11 Overdenture attachment systems with reduced height that can adapt to the different tissue heights surrounding each implant are needed to maintain sufficient material thickness on the base while limiting fractures.12 Advances in attachment systems with extended pivoting range allow for restoration of non-parallel implants with up to 20 degrees angulation.13 This calculates to an extensive 40 degrees of divergence between two implants. Complete digital customization of the overdenture abutments is possible for full customization in compromised cases where 3D implant positions are less than ideal.
Self-cured composite luting materials for capturing the female attachments into resin or PMMA dentures are safe and convenient for intraoral use, as direct pickup is more accurate than an indirect method.14
Full-Arch Implant-Supported Dental Prosthesis
Replacement of missing teeth with a full-arch fixed implant-supported dental prosthesis is a highly desirable option for most edentulous patients seeking dental treatment. Four dental implants distributed along the edentulous arch and a hybrid prosthesis with a titanium framework and acrylic denture teeth is a cost-effective solution in many clinical situations.15 Bone in the edentulous maxilla is less dense compared to the mandible. A rigid prosthesis material and more dental implants can compensate for the lower density.16 A CAD/CAM-fabricated full-arch zirconia implant-supported dental prosthesis requires a passive fit.17 Traditionally, the open-tray impression technique with splinted impression copings with a low-shrinkage modeling resin and a verification jig has provided clinically acceptable marginal adaptation (Figure 10).18 The latest generation of intraoral scanners with confocal microscopy seem to offer a viable alternative for full-arch implant impressions.19 3D-printed models with embedded digital analogs can also replicate the intraoral scan data accurately when specific 3D-printing protocols are followed and quality control is maintained (Figure 11).
Photogrammetry
Photogrammetry technology can be used to create a 3D object from 2-dimensional (2D) images. Specific scan bodies with optical markers combined with 2D photographs from a digital camera are used to digitize the implant position. These systems are capable of transferring only the 3D implant positions. Therefore, an IOS would still be needed for digitalization of the soft tissues. Scientific evidence is limited to case reports and in vitro studies reporting contradictory results.20-23
Clinical Case: Full-Arch Restoration
A female patient presented for implant therapy for her maxillary arch. After extractions of failing dentition, six implants were placed, and a PMMA immediately loaded provisional restoration was delivered the day of surgery. After an osseointegration period, full-arch intraoral scans of the provisional restoration were made for maxillo-mandibular records.
Following removal of the provisional, healing abutments were selected from the software's digital library for soft-tissue scanning and placed (Figure 12), and a gingiva scan was made. Scan posts were placed over the multi-unit abutments (Figure 13); if the location is subgingival, placement can be verified radiographically to confirm proper seating. Photogrammetry impressions were made, and data was merged in CAD software for the design and milling of a full-arch zirconia restoration (Figure 14 and Figure 15). The "APC" concept, which includes three practical steps-(A) air-particle abrasion, (P) zirconia primer, and (C) adhesive composite resin-was used for bonding to the ti-bases.24,25
Conclusions
Digital dentistry offers a shorter turnaround time than conventional procedures when needing to fabricate new or replace existing dentures. Dentures can be fabricated following analog or digital clinical workflows.Monolithic 3D-printed dentures may serve as an alternative for immediate dentures; however, long-term data is limited.
Mandibular overdentures with two non-splinted implants and maxillary overdentures with four non-splinted implants with a metal reinforcement have shown lower complication rates.26 A prosthetic space of 10 mm is needed.
Intraoral scanners with confocal microscopy technology seem to be viable for making full-arch implant impressions. Photogrammetry, used to create a 3D object from 2D images, has limited scientific evidence and the use of an intraoral scanner is still needed as part of the workflow.
Acknowledgment
The authors thank Sivothayan Sevvanthiraja, DMD, Thomas Yoo, DMD, and Sooryung Ann, CDT, for their contributions to this article on the clinical cases and research.
About the Authors
Julian Conejo, DDS, MSc
Assistant Professor, Clinical Restorative Dentistry, and Director, Chairside CAD/CAM Dentistry, Department of Preventive and Restorative Sciences, University of Pennsylvania School of Dental Medicine, Philadelphia Pennsylvania
Pablo Atria, DDS, MSc
Assistant Professor, Department of Biomaterials, College of Dentistry, Universidad de Los Andes, Santiago, Chile; Graduate Assistant, Grossman School of Medicine, New York University, New York, New York
Luciano Retana, DDS, MSc, CDT
Clinical Assistant Professor, Prosthodontics Department, Louisiana State University School of Dentistry, New Orleans, Louisiana
Kushaldeep Fnu, BDS, MDS
Resident, Advanced Prosthodontics Program, Department of Preventive and RestorativeSciences, University of Pennsylvania School of Dental Medicine, Philadelphia Pennsylvania
Kenneth Kent, DMD
Associate Professor, Clinical Restorative Dentistry, Department of Preventive and Restorative Sciences, University of Pennsylvania School of Dental Medicine, Philadelphia Pennsylvania
Markus B. Blatz, DMD, PhD
Professor of Restorative Dentistry, Chair, Department of Preventive and Restorative Sciences, and Assistant Dean, Digital Innovation and Professional Development, University of Pennsylvania School of Dental Medicine, Philadelphia Pennsylvania
Queries to the author regarding this course may be submitted to authorqueries@aegiscomm.com.
References
1. American College of Prosthodontics. Facts & Figures. ACP website. https://www.gotoapro.org/facts-figures/. Accessed September 28, 2021.
2. Goodacre CJ, Goodacre BJ, Baba NZ. Should digital complete dentures be part of a contemporary prosthodontic education? J Prosthodont. 2021;30(S2):163-169.
3. Baba NZ, Goodacre BJ, Goodacre CJ, et al. CAD/CAM complete denture systems and physical properties: a review of the literature. J Prosthodont. 2021;30(S2):113-124.
4. Lee DJ, Saponaro PC. Management of edentulous patients. Dent Clin North Am. 2019;63(2):249-261.
5. Anadioti E, Musharbash L, Blatz MB, et al. 3D printed complete removable dental prostheses: a narrative review. BMC Oral Health. 2020;20(1):343.
6. Goldstein G, Kapadia Y, Campbell S. Complete denture occlusion: best evidence consensus statement. J Prosthodont. 2021;30(S1):72-77.
7. St George G, Hussain S, Welfare R. Immediate dentures: 1. Treatment planning. Dent Update. 2010;37(2):82-91.
8. Tripathi A, Singh SV, Aggarwal H, Gupta A. Effect of mucostatic and selective pressure impression techniques on residual ridge resorption in individuals with different bone mineral densities: a prospective clinical pilot study. J Prosthet Dent. 2019;121(1):90-94.
9. Latham J, Ludlow M, Mennito A, et al. Effect of scan pattern on complete-arch scans with 4 digital scanners. J Prosthet Dent. 2020;123(1):85-95.
10. van Meegen HG, Kalk W. Improvement of a removable complete denture by relining or rebasing [article in Dutch]. Ned Tijdschr Tandheelkd. 2011;118(11):545-551.
11. Gibreel MF, Khalifa A, Said MM, et al. Biomechanical aspects of reinforced implant overdentures: a systematic review. J Mech Behav Biomed Mater. 2019;91:202-211.
12. Carpentieri J, Greenstein G, Cavallaro J. Hierarchy of restorative space required for different types of dental implant prostheses. J Am Dent Assoc. 2019;150(8):695-706.
13. Shah K, Yilmaz B, McGlumphy E. Fabrication of a mandibular implant-supported overdenture with a new attachment system: a review of current attachment systems. Int J Prosthodont. 2017;30(3):245-247.
14. Cakarer S, Can T, Yaltirik M, Keskin C. Complications associated with the ball, bar and Locator attachments for implant-supported overdentures. Med Oral Patol Oral Cir Bucal. 2011;16(7):e953-e959.
15. Maló P, de Araújo Nobre M, Lopes A, et al. The All-on-4 treatment concept for the rehabilitation of the completely edentulous mandible: a longitudinal study with 10 to 18 years of follow-up. Clin Implant Dent Relat Res. 2019;21(4):565-577.
16. Fuster-Torres MÁ, Peñarrocha-Diago M, Peñarrocha-Oltra D, Peñarrocha-Diago M. Relationships between bone density values from cone beam computed tomography, maximum insertion torque, and resonance frequency analysis at implant placement: a pilot study. Int J Oral Maxillofac Implants. 2011;26(5):1051-1056.
17. Blatz MB, Vonderheide M, Conejo J. The effect of resin bonding on long-term success of high-strength ceramics. J Dent Res. 2018;97(2):132-139.
18. Ercoli C, Geminiani A, Feng C, Lee H. The influence of verification jig on framework fit for nonsegmented fixed implant-supported complete denture. Clin Implant Dent Relat Res. 2012;14 suppl 1:e188-e195.
19. Kim RJY, Benic GI, Park JM. Trueness of ten intraoral scanners in determining the positions of simulated implant scan bodies. Sci Rep. 2021;11(1):2606.
20. Molinero-Mourelle P, Lam W, Cascos-Sánchez R, et al. Photogrammetric and intraoral digital impression technique for the rehabilitation of multiple unfavorably positioned dental implants: a clinical report. J Oral Implantol. 2019;45(5):398-402.
21. Peñarrocha-Oltra D, Agustín-Panadero R, Pradíes G, et al. Maxillary full-arch immediately loaded implant-supported fixed prosthesis designed and produced by photogrammetry and digital printing: a clinical report. J Prosthodont. 2017;26(1):75-81.
22. Revilla-León M, Rubenstein J, Methani MM, et al. Trueness and precision of complete-arch photogrammetry implant scanning assessed with a coordinate-measuring machine. J Prosthet Dent. 2021;18:S0022-3913(21)00280-8.
23. Revilla-León M, Att W, Özcan M, Rubenstein J. Comparison of conventional, photogrammetry, and intraoral scanning accuracy of complete-arch implant impression procedures evaluated with a coordinate measuring machine. J Prosthet Dent. 2021;125(3):470-478.
24. Blatz MB, Alvarez M, Sawyer K, Brindis M. How to bond zirconia: the APC concept. Compend Contin Educ Dent. 2016;37(9):611-617.
25. Conejo J, Kobayashi T, Anadioti E, Blatz MB. Performance of CAD/CAM monolithic ceramic implant-supported restorations bonded to titanium inserts: a systematic review. Eur J Oral Implantol. 2017;10 suppl 1:139-146.
26. Wismeijer D, Casentini P, Gallucci G, Chiapasco M. ITI Treatment Guide, Volume 4: Loading Protocols in Implant Dentistry - Edentulous Patients. Berlin, Germany: Quintessence Publishing; 2010.