You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
The question of whether a restorative dentist should restore a badly broken-down endodontically treated maxillary anterior tooth or extract and replace it with a dental implant is extremely difficult to answer. This is particularly so in light of the literature showing that a well-placed implant in an acceptable site with adequate surrounding bone can be restored predictably to look esthetically pleasing and function well for many years.1 Abutment and restorative materials have progressed over the years, and today clinicians are capable of producing excellent implant restorations.
Restorative dentists follow the Hippocratic Oath to "first, do no harm." In 1952, DeVan stated eloquently, "Our objective should be the perpetual preservation of what remains rather than the meticulous restoration of what is missing."2 Often, when faced with the pressure to satisfy patients, restorative dentists attempt to save teeth that should not be saved. Dental implants, dentists are taught, are not teeth; they are replacements for teeth. However, implants frequently can provide a better solution to a given problem, as many times clinicians' attempts to restore a badly dilapidated tooth can result in an unacceptable esthetic outcome.
A Challenging Situation
The compromised maxillary anterior tooth is often the most challenging situation a dentist faces. The decision to either restore or extract such a tooth should be based on set criteria and scientific research; however, many times this all-important decision is based mostly on the dentist's clinical experience and the patient's demands. This decision can be complicated, and as the literature suggests, the 74-month survival rate of a restored, endodontically treated tooth is 72.7%.3 The literature is difficult to decipher when it comes to actual survival rates in these cases because of the multitude of variables that come into play. Indeed, survival rates in several studies are contradictory, with some stating high rates and some relatively low.4-6
The clinician must decide whether to restore the badly damaged tooth, extract the tooth and place an implant, or extract the tooth and replace it with either a bonded or conventional fixed partial denture (FPD). The purpose of this article is to provide simple, straightforward criteria for clinicians to follow when making this difficult decision. The clinician's ultimate goal is to provide the patient with the most predictable and long-lasting restoration possible, one that satisfies functional and esthetic requirements, as well as the patient's desires.
Failure of a restoration in the esthetic zone can be subjective; while it may be a functional success, it may be deemed by the patient an esthetic failure regardless of the type of post-and-core used, whether or not extrusion or crown lengthening was done, or whether the emergence profile is similar to the surrounding teeth. Because esthetics are subjective and personal, a restoration, despite having excellent function, could be considered a failure, and this is something the clinician may have little or no control over. For example, often times an endodontically treated root will turn dark over time, and if the tissue is thin the darkness will show through well after the tooth was restored.
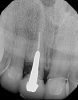
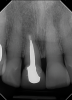
In the case presented in Figure 1 and Figure 2, the author based the decision to restore a badly compromised maxillary central incisor on his clinical experience and the patient's desire to keep the tooth, and while the restoration lasted several years, the esthetic result turned out to be poor due to the gray show-through at the gingival area and deep below the tissue from the root (Figure 2). The literature has indicated that this dark discoloration may be due to the use of certain intracanal medicaments during the root canal procedures, including some antibiotic pastes and/or liquids, or possibly the previous use of metallic restorative material in the canal.7,8 Removal of this discoloration is difficult and Zimmerli et al showed in a literature review that different bleaching techniques offer limited success and a high incidence of the discoloration returning.9
There are two important points that can be gleaned from this case when considering the restoration of compromised teeth. The first is whether the esthetic failure caused by the gray show-through could have been avoided if the tooth had been replaced with a dental implant. If the darkness was caused by the discolored root, the better option may have been to extract the tooth and graft the site; with thickened tissue and adequate bone, an implant may have been able to have been placed without any residual dark show-through. And secondly, how much should patients' desires influence, or even dictate, treatment options? While these questions may never be definitively answered, there are several criteria based on sound research that are crucial in a clinician's decision-making process.
Criteria for Decision-Making
Prognosis
In situations where the prognosis for a badly damaged tooth is poor, or the existing post-and-core is failing, it is best to make the definitive decision to extract the tooth before more extensive damage and bone loss can occur, thus allowing for the successful placement and restoration of an implant and restoration of adjacent teeth and the surrounding periodontium (Figure 3 through Figure 5).10 If the attempt to restore the tooth ultimately proves to be unsuccessful over time, and the decision to extract the tooth is made too late, the potential implant site may be compromised, especially if there is a root fracture with resulting loss of bone. Eventually, this can be a devastating outcome for the patient. If the site is compromised, the esthetic results of the final restoration will be poor, often necessitating the use of gingival-colored porcelain. While this material can be utilized with success, it is generally considered a compromised treatment outcome with implants (Figure 6 and Figure 7). When the clinician fails to make gingival-colored porcelain match the surrounding periodontium the results can be catastrophic (Figure 8).
Cost
Cost is typically a primary factor in the decision process. The costs/benefits of every restorative procedure must always be weighed out, and clinicians should help patients make predictable decisions that they can afford. If the 5-year prognosis of the tooth in question is poor, then it does not make sense to have the patient incur the expense of multiple procedures, and the tooth should be extracted. Once cost-effectiveness has been discussed, the simple flowchart shown in Figure 9 can be referenced to assist clinicians organize their thoughts while assessing the damaged tooth, and it provides a checklist for making restorative decisions.
Smile Line and Amount of Tooth Structure
Dentistry should strive to restore teeth and mimic nature, and the patient's smile line remains one of the most critical variables in the "restore or replace" decision process. The higher the smile line and the more gingiva that is displayed during a relaxed smile and normal speech, the more critical it is that the restorative decisions have predictable outcomes in mimicking nature. Compromised esthetic results in the patient with a high smile line are more likely to be problematic than in a patient with a low smile line. A low smile line offers a buffer if the restoration fails to mimic nature and has minor flaws.
Therefore, the two most important criteria that must be considered when deciding to restore an endodontically treated maxillary anterior tooth are the smile line and the amount of remaining tooth structure. The smile line and the display of the tooth in question are priorities when making decisions. Certainly, when a tooth is covered by the lip during rest, the decision-making process is easier. The more a tooth shows, ie, in a patient with a high lip line, the more predictable the restoration needs to be from an esthetic standpoint, and for the discerning patient even the smallest esthetic compromise may be considered a disappointment. With the full display of the tooth during normal and accentuated function, often the slightest imperfections can be deemed a failure.
If the patient has a low smile line, small compromises may be acceptable, and in such a case the decision is based more on the amount of remaining tooth structure and how many tooth walls are available for a ferrule effect, if a post is necessary. If inadequate tooth structure remains, other treatment options could be considered, such as crown lengthening or orthodontic extrusion, to improve the amount of restorable tooth structure. Pantaleón et al showed in an extensive literature review that 4 mm of remaining tooth structure is necessary for predictable long-term results.11 With a low lip line, problems such as slight mismatches in emergence profile, which occur when a tooth is extruded and a tapered root is exposed, may be more acceptable when covered during normal and accentuated function of the lip. With the low lip line, the remaining tooth structure is the primary consideration, and when there is adequate tooth structure for a post and buildup, the tooth should be restored. If there is inadequate tooth structure and the other aforementioned treatment options, ie, crown lengthening or orthodontic extrusion, are not feasible, the author suggests the tooth should be extracted and replaced with an implant or FPD. Proper site enhancement procedures should then ensue to optimize the edentulous area for an acceptable pontic or implant.
Phenotype
Although it is not included in the treatment flowchart (Figure 9) for the sake of simplicity, the phenotype of the surrounding tissues is critical. It has been suggested that long-term restorative success with both teeth and implants in thin phenotype is more difficult than in thick phenotype.10,12 This factor should always be considered by the clinician; however, the author believes that the smile line is more critical in determining whether or not a tooth should be extracted. Even though attaining success is easier with a thick phenotype versus a thin phenotype, having the former condition still does not assure total success, and in a patient with a high smile line even thick tissue will not necessarily guarantee a successful outcome.
With a thick phenotype, teeth are generally square in shape, and the emergence profile of the final restoration is much simpler to achieve than with a thin phenotype and tapered teeth.13 With tapered teeth and thin tissue, the clinician might be better off extracting the remaining tooth early and focusing on properly preparing the implant site and optimizing the available bone.
Restorative Options
For a patient who has a low smile line and adequate tooth structure, one choice to restore a maxillary anterior tooth is a prefabricated metallic parallel post.14 In an extensive literature review, Heydecke showed a 93% success rate over 3 years with this technique.15 Alternatively, one can utilize a split-shank parallel-sided threaded post and composite build-up, a custom cast post made from precious or semiprecious metal, or a custom post-and-core made with lithium disilicate or zirconia.16 Active, threaded posts have been reported in the literature to have low survival rates and increased stress to the dentinal walls of the remaining root.17 Thorsteinsson noted that Flexi-posts® were shown to have reduced stresses in in vitro studies, but parallel, nonthreaded posts showed the least amount of internal stress.18 While higher survival rates have been reported when either prefabricated, passive parallel posts or custom cast posts are utilized, design of the post-and-core has been shown to be critical. It has been demonstrated that 4 mm to 5 mm of remaining tooth structure utilized with a good ferrule helps ensure long-term success.19-21 Tan et al showed that a ferrule on anything less than 4 mm of remaining tooth structure is no more resistant to fracture than having no ferrule at all.22
Coronal seal and maintaining 5 mm of gutta percha in the apical portion of the canal have also been shown to be critical, along with good coronal seal of the final restoration.4,5,11,23 Properly restored endodontically treated teeth can last many years when appropriately treatment-planned. Figure 10 and Figure 11 demonstrate a case in which tooth No. 8 was restored with a cast post-and-core and a properly fitted crown. The images show a 24-year follow-up on the tooth.
Equally important, even in cases where the patient has a low smile line, 4 mm of remaining tooth structure, and a well-designed post-and-core, poor coronal seal due to a clinically unacceptable crown marginal seal can still eventually lead to failure.23 Good judgment and sound principles are not enough to overcome poor restorative technique.
When less than 4 mm of tooth structure is remaining other restorative options are available for clinicians to consider. Orthodontic extrusion and/or surgical crown lengthening may be used to increase the amount of remaining tooth structure and re-establish the biologic width. The literature has shown that orthodontic extrusion with or without the addition of surgical crown lengthening may result in successful restorations, both esthetically and functionally.24 However, when considering either of these options, a thorough knowledge of the anatomy of the tooth and the root anatomy below the gingival attachment is essential, as the resultant exposed tooth may result in an emergence profile that is narrower than that of the adjacent teeth, thus creating an even greater esthetic challenge.25-27
When the clinician has exhausted all of the restorative options for a compromised endodontically treated anterior tooth, or the patient has a high smile line, the decision to extract and replace the tooth with either an implant or FPD should be made. For the purposes of this article it is assumed that the future site will be optimized for either a pontic if an FPD is planned or an implant. The remaining root may be utilized further, and optimization of the site can be accomplished with extrusion of the root to regenerate bone.28-30
Conclusion
While the decision to extract an endodontically treated maxillary anterior tooth can be a difficult one, the flowchart presented in Figure 9 is designed to assist clinicians in making decisive recommendations to patients. Recommendations should be intended to prevent further loss of bone in a potential implant site. These decisions need to be made in a timely fashion to improve the chances of optimized results. When a compromised tooth begins to show bone loss, as evidenced by a deep probing and loose crown, restorative decisions must be expedient (Figure 12 and Figure 13).
The lip line is critical in the decision process, and the clinician must inform the patient of the possibility of the appearance of undesirable subtle darkness at the gingival area if a wrong decision is made. While an endodontically treated tooth can be predictably restored and last a long time utilizing sound principles and clinical experience and skill, the time and money spent on restoring the tooth in a patient with a high smile line may not be ideal. Extraction, site development, and implant placement may be the better option.
Perhaps when DeVan stated that dentists' mission is to "preserve what remains" he was not necessarily referring to just saving teeth, but making informed choices that may include extracting teeth to preserve valuable bone for implants, particularly when a patient has a high smile line that may reveal small imperfections in the restorations. While it is true that implants are not teeth but replacements for teeth, they have proven to be sound substitutes and are often the better choice for the patient when considering cost of treatment, length of time for treatment, and long-term predictability.
About the Author
Gary Solnit, DDS, MS
Fellow, International Team for Implantology; Private Practice in Prosthodontics, Beverly Hills, California
Queries to the author regarding this course may be submitted to authorqueries@aegiscomm.com.
References
1. Belser UC, Martin W, Jung R, et al. ITI Treatment Guide. Volume 1. Implant Therapy in the Esthetic Zone - Single-Tooth Replacements. Quintessence Publishing; 2007.
2. DeVan MM. The nature of the partial denture foundation: suggestions for its preservation. J Prosthet Dent. March 1952;2(2):210-218.
3. Chatzopoulos GS, Koidou VP, Lunos, S, Wolff LF. Implant and root canal treatment: survival rates and factors associated with treatment outcome. J Dent. 2018;71:61-66.
4. Martino N, Truong C, Clark AE, et al. Retrospective analysis of survival rates of post-and-cores in a dental school setting. J Prosthet Dent. 2020;123(3):434-441.
5. Ibrahim AM, Richards LC, Berekally TL. Effect of remaining tooth structure on the fracture resistance of endodontically-treated maxillary premolars: an in vitro study. J Prosthet Dent. 2016;115(3):290-295.
6. Lazari PC, de Carvalho MA, Del Bel Cury AA, Magne P. Survival of extensively damaged endodontically treated incisors restored with different types of posts-and-core foundation restoration material. J Prosthet Dent. 2018;119(5):769-776.
7. Afkhami F, Elahy S, Nahavandi AM, et al. Discoloration of teeth due to different intracanal medicaments. Restor Dent Endod. 2019;44(1):e10.
8. Afkhami F, Elahy S, Mahmoudi-Nahavandi A. Spectrophotometric analysis of crown discoloration following the use of silver nanoparticles combined with calcium hydroxide as intracanal medicament. J Clin Exp Dent. 2017;9(7):e842-e847.
9. Zimmerli B, Jeger F, Lussi A. Bleaching of nonvital teeth. A clinically relevant literature review. 2010;120(4):306-320.
10. Chappuis V, Araujo MG, Buser, D. Clinical relevance of dimensional bone and soft tissue alterations post-extraction in esthetic sites. Periodontol 2000. 2017;73(1):73-83.
11. Pantaleón DS, Morrow BR, Cagna DR, et al. Influence of remaining coronal tooth structure on fracture resistance and failure mode of restored endodontically treated maxillary incisors. J Prosthet Dent. 2018;119(3):390-396.
12. Wang IC, Barootchi S, Tavelli L, Wang HL. The peri-implant phenotype and implant esthetic complications. Contemporary review. J Esthet Restor Dent. 2021;33(1):212-223.
13. Malpartida-Carillo V, Tinedo-Lopez PL, Guerrero ME, et al. Periodontal phenotype: a review of historical and current classifications evaluating different methods and characteristics. J Esthet Restor Dent. 2021;33(3):432-445.
14. Fadag A, Negm M, Samran A, et al. Fracture resistance of endodontically treated anterior teeth restored with different post systems: an in vitro study. Eur Endod J. 2018;3(3):174-178.
15. Heydecke G, Peters MC. The restoration of endodontically treated, single-rooted teeth with cast or direct posts and cores: a systematic review. J Prosthet Dent. 2002;87(4):380-386.
16. Setzer FC, Kim S. Comparison of long-term survival of implants and endodontically treated teeth. J Dent Res. 2014;93(1):19-26.
17. Kahn FH, Rosenberg PA, Schulman A, Pines M. Comparison of fatigue for three prefabricated threaded post systems. J Prosthet Dent. 1996;75(2):148-153.
18. Thorsteinsson TS, Yaman P, Craig RG. Stress analyses of four prefabricated posts. J Prosthet Dent. 1992;67(1):30-33.
19. Meng QF, Chen LJ, Meng J, et al. Fracture resistance after simulated crown lengthening and forced tooth eruption of endodontically-treated teeth restored with a fiber post-and-core system. Am J Dent. 2009;22(3):147-150.
20. Meng Q, Ma Q, Wang T, Chen Y. An in vitro study evaluating the effect of ferrule design on the fracture resistance of endodontically treated mandibular premolars after simulated crown lengthening or forced eruption methods. BMC Oral Health. 2018;18(1):83.
21. Juloski J, Radovic I, Goracci C, et al. Ferrule effect: a literature review. J Endod. 2012;38(1):11-19.
22. Tan PL, Aquilino SA, Gratton DG, et al. In vitro fracture resistance of endodontically treated central incisors with varying ferrule heights and configurations. J Prosthet Dent. 2005;93(4):331-336.
23. Mannocci F, Bhuva B, Stern S. Restoring teeth following root canal re-treatment. Endodontic Topics. 2011;19(1):125-152.
24. Pham HT, Nguyen PA, Pham TAV. Periodontal status of anterior teeth following clinical crown lengthening by minimally traumatic controlled surgical extrusion. Dent Traumatol. 2018;34(6):455-463.
25. Scholtes E, Suttorp CM, Lohmanns BA, et al. Combined orthodontic, surgical, and restorative approach to treat a complicated crown-root fracture in a maxillary central incisor. Am J Orthod Dentofacial Orthop. 2018;154(4):570-582.
26. Esposito S. Management of the dentogingival complex after forced eruption: a case report. Gen Dent. 2003;51(1):58-60.
27. Angerame D, de Biasi M, Kalaj B, Maglione M. Surgical extrusion: a dental technique. J Prosthet Dent. 2021;125(1):23-28.
28. Hasson JN, Hasson B. Implant site development by orthodontic forced eruption for esthetic restoration of adjacent implants. Clin Adv Periodontics. 2016;6(3):146-152.
29. Lin IP, Hsaing-Hua Lai E, Zwei-Chieng Chang J, Wang CY. Staged orthodontic treatment in preparation for immediate implant placement: a clinical report with a 5-year follow-up. J Prosthet Dent. 2019;122(6):503-509.
30. Buskin R, Castellon P, Hochstedler JL. Orthodontic extrusion and orthodontic extraction in presprosthetic treatment using implant therapy. Pract Periodontics Aesthet Dent. 2000;12(2):213-219.