You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
The primary esthetic goal of any dental restoration is to not only match the optical characteristics of the natural tooth structures but also to create integration into the surrounding soft tissues. A major challenge in esthetic dentistry is successfully achieving a pleasing appearance along with ideal harmony among the teeth, soft tissues, and patient's face.
In the past decade, digitalization of patients' intra- and extraoral structures for facially driven treatment planning has gained popularity among clinicians. This approach has facilitated improved interaction among specialists and enabled clinicians to more clearly and effectively explain different treatment plan options to patients.
Monolithic restorations fabricated with CAD/CAM technologies are used frequently because of their clinical reliability, cost efficiency, and reduced production time.1 Conversely, handmade layered restorations constructed using multiple types of dentin and enamel porcelain powders as well as internal and external stains under multiple firing cycles are considered high-end restorations and are associated with higher cost and greater time consumption.2 Also, successfully managing material thicknesses, tooth preparations, and use of the correct method for shade selection is paramount to achieve clinical success. Tooth structure plays an important role when deciding the correct thickness of materials and, thus, how much enamel and dentin will be preserved.3
The combination of different digital technologies, such as 3D printing and CAD/CAM, allows clinicians to improve their workflow and integrate technologies to achieve not only a successful treatment plan but also better communication with the patient. Moreover, the increase in popularity of these technologies has led to the development of multiple hardware and software products that provide a number of enhanced capabilities. These include the combining of intraoral and extraoral acquisition; improved communications between various manufacturers and developers; and the opportunity to export digital files (that are now open to the users) and import them in a wide variety of design software, expanding the available technologies to obtain the desired final outcome.4
Available computer design software for dental applications can simplify the task of mimicking tooth anatomy, shape, and texture. Familiarity with the benefits and disadvantages of these tools, as well as knowing the possibilities of mixing their applications in different steps of the process, can allow clinicians to achieve better results in a shorter time than conventional means without compromising the quality of the final restorations.5
All of these factors are considerations in the current shift in dentistry from analog to digital workflows in performing prosthetic treatments. Thus, the objective of this article is to demonstrate a technique that combines the use of different CAD/CAM software systems to enhance the macro- and micro-anatomy of digital designs, reduce post-milling characterization times, and achieve excellent esthetic results.6
Enhancing Tooth Morphology and Surface Texture
This technique uses the design from any 3D software program to enhance tooth morphology and surface texture without having to revert back to the initial scan when major changes are needed. What the authors call the "ReShape" concept can be used to enhance single-unit restorations, short-span fixed dental prostheses, full-arch monolithic restorations, and digital dentures. This technique is especially valuable for fabrication of full-arch restorations when, very often, the interproximal areas and the design of the connectors do not create a natural esthetic morphology. Typically, a milled prototype is recommended for completely edentulous cases. A limitation of this technique is that the emergence profile of the initial design cannot be modified.
Case Report
A 40-year-old male patient presented with severe teeth discolorations. He stated that other family members had the same type of stains. After clinical and radiographic evaluation, the diagnosis was severe fluorosis and generalized periodontitis with probing depths of 4 mm to 6 mm as well as partial edentulism with absence of mandibular incisors (Figure 1).
Initial periodontal therapy comprised scaling and root planing. The patient was reevaluated 4 months later, and his periodontal health had improved. After the patient was presented with different treatment options, he elected ceramic restorations to close his diastemas and mask tooth discoloration of the maxillary anterior teeth and a partial removable prosthesis to replace the missing mandibular incisors; he refused orthodontics, soft-tissue grafting, and implant therapy.
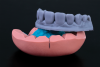
Intraoral (Figure 1) and extraoral photographs revealed the severity of the periodontitis, with soft-tissue loss and diastemas prevalent. Intraoral scans were taken, and a 3D smile analysis was performed with the use of an application (Figure 2). (The authors used DSDApp® [DSD - Digital Smile Design]. A similar app that could be used for this purpose is Smilecloud Biometrics® [Smilecloud].) A 3D-printed model from the digital wax-up made on the app was used to create two silicone indexes, one to serve as a tooth reduction guide and the other for fabrication of the provisional restorations (Figure 3).
Due to severe discolorations penetrating into the dentin and extensive mesiodistal diastemas, the maxillary central incisors were prepared for full-coverage restorations. With such substantial spaces, a 0.5 mm subgingival margin was planned, which would help support the soft tissue and reduce black triangles. Such a margin would also help reduce potential overcontouring of the final restorations due to the absence of vertical space availability in the emergence profile.
Maxillary lateral incisors and canine teeth were prepared for facial laminate veneers using a conservative approach with cutting burs of 0.3 mm depth, which facilitated the conservation of enamel on this type of preparation for partial-coverage restorations. Subsequently, a digital intraoral final impression was made using a powder-free scanner and exported to the laboratory through the scanner software-specific connection portal.
The restorations were initially designed in one software program (InLab 19, Dentsply Sirona) (Figure 4 and Figure 5) and then exported into another (DentalCAD 2.4 Plovdiv, Exocad) for "reshaping" (Figure 6 through Figure 10). (Other applicable software containing natural tooth libraries includes Trios® Design Studio, 3Shape.)
The step-by-step process is as follows: In the dental CAD software, a new case is created and the elements that will be modified are selected as "pontics." Next, the previously designed file from any 3D software is imported as "model" in STL format (Figure 6 and Figure 7). If no occlusal modifications are needed and only the facial surface of the previous design will be modified, the opposing model should not be imported. Then, in the design phase, the new tooth with natural surface texture is selected from the preferred library within the dental CAD software. The position of the selected teeth is adjusted over the initial design, and final adjustments are then made within the altered surface digitally, using design tools in the software. All teeth can be modified individually (Figure 8 and Figure 9). Next, the root portions of the selected teeth are removed by editing the mesh (Figure 10). Lastly, once the new design is finished, a new STL file is created and exported to any CAM software for production of the final restorations.
Crowns and veneers with natural texture and contours were milled from zirconia-reinforced lithium-silicate ceramic blocks, and a stain/glaze technique was applied.
After try-in, the internal surfaces of the restorations were etched with hydrofluoric acid for 20 seconds, as per manufacturer's instructions, and subsequently cleaned in an ultrasonic distilled water bath for 5 minutes. Adhesive cementation was performed for a dual-cure, color-stable dentin bonding resin cement, clear shade, following manufacturer's recommendations. Final intraoral and extraoral images (Figure 11 through Figure 14) show the integration of the restorations to the soft tissues with natural morphology and texture while also demonstrating dentofacial harmony.
Discussion
The present technique describes a simple step-by-step protocol for combining two different software programs to obtain restorative treatment that presents ideal anatomy, surface texture, and esthetics. While traditional approaches require the use of conventional impression materials, stone casts, wax-ups, and handmade dental ceramics with their respective anatomical and optical characterizations, the current technique uses intraoral scanning, digital design, and milling. The ability to use natural tooth shapes from dental scan libraries within design software and modify these designs with specific tools in the same or a different software program decreases working times without compromising the final result.
In addition to higher patient acceptance,7 one of the biggest advantages of digital dentistry is that it enables clinicians to achieve favorable and highly reproducible clinical results with less chairtime than conventional means.8 As a result, these technologies have been used for a wide variety of clinical applications, including guided implant surgeries, digital wax-ups, orthodontic planning and treatment, and others.5,9-11
The continuous development of digital technologies has led to an increase in the variety of restorative materials. In this case, a zirconia-reinforced lithium-silicate ceramic was the material of choice. It offers ideal properties for monolithic restorations due to its mechanical and optical characteristics.12,13 It has been reported that the pronounced translucency of this material increases its chameleon effect and improves shade adaptation.14
A systematic review reported that esthetics with ceramic veneers were good over time, patient satisfaction was high, and retention rate was excellent after 10 years.15 Moreover, the material used in this case, zirconia-reinforced lithium-silicate ceramic, presents natural opalescence, fluorescence, and chameleon effect with excellent mechanical properties, such as 370 MPa flexural strength after milling and firing.16,17
The high initial cost for the necessary digital equipment remains a drawback for many clinicians. However, as the shift toward digital dentistry continues to proliferate, digital technologies and equipment can be expected to become increasingly cost-effective in the long term.
Conclusion
The technique described in this article should be considered as another option for clinicians to take advantage of digital dentistry and available software programs to facilitate esthetic success in demanding cases. Among the benefits of this technique are enhanced final optical properties and macro- and micro-anatomical characteristics.
About the Authors
Julian Conejo, DDS, MSc
Assistant Professor, Clinical Restorative Dentistry, and Director, Chairside CAD/CAM Dentistry, Department of Preventive and Restorative Sciences, University of Pennsylvania School of Dental Medicine, Philadelphia, Pennsylvania
Telmo Santos
Chief Executive Officer, Coterc Digital Lab, Belo Horizonte, Minas Gerais, Brazil
Pablo J. Atria, DDS, MSc
Assistant Professor, Department of Biomaterials, College of Dentistry, Universidad de Los Andes, Santiago, Chile; Graduate Assistant, Grossman School of Medicine, New York University, New York, New York
Aledy Moreta, DMD
Private Practice, Philadelphia, Pennsylvania
Markus Blatz, DMD, PhD
Professor of Restorative Dentistry, Chair, Department of Preventive and Restorative Sciences, and Assistant Dean, Digital Innovation and Professional Development, University of Pennsylvania School of Dental Medicine, Philadelphia, Pennsylvania
Queries to the author regarding this course may be submitted to authorqueries@aegiscomm.com.
References
1. Wittneben JG, Wright RF, Weber HP, Gallucci GO. A systematic review of the clinical performance of CAD/CAM single-tooth restorations. Int J Prosthodont. 2009;22(5):466-471.
2. Yuce M, Ulusoy M, Turk AG. Comparison of marginal and internal adaptation of heat-pressed and CAD/CAM porcelain laminate veneers and a 2-year follow-up. J Prosthodont. 2019;28(5):504-510.
3. Coachman C, Gurel G, Calamita M, et al. The influence of tooth color on preparation design for laminate veneers from a minimally invasive perspective: case report. Int J Periodontics Restorative Dent. 2014;34(4):453-459.
4. Rekow ED. Digital dentistry: the new state of the art - is it disruptive or destructive? Dent Mater. 2020;36(1):9-24.
5. Malta Barbosa J, Tovar N, Tuesta PA, et al. Scan-layered reconstructions: a pilot study of a nondestructive dental histoanatomical analysis method and digital workflow to create restorations driven by natural dentin and enamel morphology. J Esthet Restor Dent. 2017;29(4):256-263.
6. Atria PJ, Sampaio CS, Hirata R, Jorquera G. Preliminary evidence for the complete digital esthetic rehabilitation treatment: case report and 1-year follow-up. J Evid Based Dent Pract. 2017;17(2):76-82.
7. Christensen GJ. Will digital impressions eliminate the current problems with conventional impressions? J Am Dent Assoc. 2008;139(6):761-763.
8. Yuzbasioglu E, Kurt H, Turunc R, Bilir H. Comparison of digital and conventional impression techniques: evaluation of patients' perception, treatment comfort, effectiveness and clinical outcomes. BMC Oral Health. 2014;14:10.
9. D'haese J, Ackhurst J, Wismeijer D, et al. Current state of the art of computer-guided implant surgery. Periodontol 2000. 2017;73(1):121-133.
10. Sampaio CS, Atria PJ. Restaurações diretas e impressões 3D: do computador ao dente. J Clin Dent Res. 2018;15(2):16-25.
11. Harrell Jr WE, Hatcher DC, Bolt RL. In search of anatomic truth: 3-dimensional digital modeling and the future of orthodontics. Am J Orthod Dentofacial Orthop. 2002;122(3):325-330.
12. Li RWK, Chow TW, Matinlinna JP. Ceramic dental biomaterials and CAD/CAM technology: state of the art. J Prosthodont Res. 2014;58(4):208-216.
13. Denry I, Kelly JR. Emerging ceramic-based materials for dentistry. J Dent Res. 2014;93(12):1235-1242.
14. Rinke S, Pabel AK, Rödiger M, Ziebolz D. Chairside fabrication of an all-ceramic partial crown using a zirconia-reinforced lithium silicate ceramic. Case Rep Dent. 2016;2016:1354186.
15. Peumans M, De Munck J, Fieuws S, et al. A prospective ten-year clinical trial of porcelain veneers. J Adhes Dent. 2004;6(1):65-76.
16. Celtra® Duo Zirconia-Reinforced Lithium Silicate (ZLS). Milford, DE: Dentsply Sirona; 2017.
17. Lawson NC, Bansal R, Burgess JO. Wear, strength, modulus and hardness of CAD/CAM restorative materials. Dent Mater. 2016;32(11):e275-e283.