You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
Patients frequently present to a dental office or clinic with a problematic, previously endodontically treated tooth. A significant challenge arises when the patient has no remembrance of how long ago the endodontic treatment was performed or who performed it. There are no past radiographs or records to reference, and a treatment assessment must be made based only on how the patient currently presents.
To determine the correct course of endodontic retreatment, the clinician needs to first make a proper pretreatment diagnosis and identify the etiology of the patient's endodontic tooth pain and/or radiographic periradicular lesion. This type of endodontic case scenario may empirically be referred to as forensic endodontics. By definition, forensic science is the collection, preservation, and analysis of scientific evidence during the course of an investigation. This article will outline the components involved in performing forensic endodontics and provide a case report describing intentional replantation surgery.
Diagnostic Tests
After reviewing the patient's medical and dental history, which includes recording blood pressure and pulse, the clinician must determine the diagnosis and etiology of the tooth pain and/or radiographic lesion before performing any type of endodontic retreatment. To determine etiology, first a pretreatment pulpal and periradicular diagnosis is obtained. This is done by listening to the patient's perception of the problem; this "chief complaint" is subjective. This is followed by the clinician performing clinical sensibility testing, which is objective, to reproduce the patient's subjective pain symptoms.1 This testing encompasses the following: (1) cold, electric pulp tester (EPT) and/or hot tests (to test pulpal status); (2) percussion and bite tests to determine the status of the periodontal ligament; (3) palpation testing to evaluate gingival tissue and cortical and trabecular bone for infection or inflammation; (4) periodontal examination that includes periodontal probings and tooth mobility evaluation; and (5) radiographic examination of current periapical film, bitewings, and/or cone-beam computed tomography (CBCT) scans.
Recording of Diagnostic Data
To properly determine the correct pretreatment pulpal and periradicular diagnosis, the clinician must obtain the correct test result data after performing the aforementioned objective tests. Then, after acquiring the correct test result data, it is important that this data be recorded in an objective, not subjective, manner. An example of subjective recording of data is to use "+" or "-" symbols when documenting the results of sensibility tests. Trying to differentiate a patient's pain level response from the symbols "++" versus "+++" can be difficult and is subjective. Also, clinicians typically are trained in dental school that if the patient does not respond to pain from testing, it should be recorded as a "-".
The recommended data recording method is the use of medical diagnostic terminology. The clinician, therefore, should use the terms "abnormal" (AB) and "within normal limits" (WNL) instead of "+" and "-", respectively, when recording palpation, percussion, and cold sensibility testing data. In addition, when recording cold sensibility testing, WNL, NR ("no response"), AB/NL ("hyper-responsive to cold that is non-lingering"), and AB/L ("hyper-responsive to cold that is lingering beyond 5 seconds") should be used. A patient response of AB/NL indicates a pretreatment pulpal diagnosis correlation to reversible pulpitis, whereas a response of AB/L denotes a pretreatment pulpal diagnosis correlation to symptomatic irreversible pulpitis.
It should be noted that the time it takes for a patient to respond to cold has no correlation to the diagnosis and, therefore, does not need to be recorded. What is important is whether a patient's response to cold is normal or hyper-responsive and whether it lingers. Also, if a tooth does not respond to cold and EPT tests, the clinician should not necessarily presume the pulp to be necrotic, because these sensibility tests stimulate only the A-delta nerve fibers and not the C-fibers of the pulp.2,3 Therefore, the pulp may still be vital due to the presence of active C-fibers. With regard to recording data for mobility and periodontal probings, numerical documentation or the use of WNL or AB terminology is appropriate.
Pulpal and Periradicular Diagnosis
The pulpal diagnosis in forensic endodontic cases is "previously treated." If the patient reports that the root canal of the tooth is sensitive to cold, it is highly unlikely that the etiology is the endodontically treated tooth, because the A-delta fibers cannot survive in a hypoxic (low-oxygen) environment.2 In such a scenario, the clinician should objectively cold test the teeth adjacent to the endodontically treated teeth. Also, if a posterior tooth is involved, the clinician should confirm with the patient that there is no referred pain from the maxilla to the mandibular jaw or vice versa due to cold stimulus. Conversely, when a patient complains of sensitivity to hot stimulus, the previously endodontically treated tooth in question should not be eliminated from etiology considerations. It has been reported that C-fibers can remain vital in the extreme apical portion of a root canal-treated tooth and, therefore, respond to a heat stimulus.4
While the pulpal diagnosis is an essential part of endodontic treatment prior to performing any root canal treatment or retreatment, a periradicular diagnosis is equally as important. A study by McCarthy et al demonstrated that patients who presented with periradicular pain were better able to localize the painful tooth (89%) in comparison to patients who presented with tooth pain without periradicular pain (30%).5 Current periradicular diagnosis terminologies are as follows6:
Symptomatic apical periodontitis: The tooth has a painful response to biting, palpation, and/or percussion; this may or may not be accompanied by radiographic changes.
Asymptomatic apical periodontitis: The tooth has no pain in response to biting, percussion, or palpation. Radiograph reveals a periradicular radiolucency.
Chronic apical abscess: Radiograph typically reveals a periradicular radiolucency. Clinically, a sinus tract is present on the gingival tissue. The draining sinus tract should be traced with a gutta-percha cone and then radiographed to confirm etiology and periodontal diagnosis.
Acute apical abscess: This is an inflammatory reaction to pulpal infection and necrosis characterized by rapid onset, spontaneous pain, extreme tenderness of the tooth to pressure, and pus formation and swelling of associated tissues. Radiographic signs of osseous resorption may be present, and the patient often may experience malaise, fever, and/or lymphadenopathy.
Effectiveness of CBCT
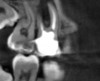
CBCT can be used to aid in further assessment of a previously endodontically treated tooth. A study by Uraba et al demonstrated that CBCT imaging is 20% more effective in detecting periapical lesions that cannot be detected on a periapical radiograph (Figure 1 and Figure 2).7 Diagnostic CBCT can provide additional information in comparison to periapical radiographs when treatment planning an endodontic retreatment case.8 The use of a limited field of view (FOV) CBCT on a patient that presents with a problem on an existing endodontically treated tooth can allow the clinician to critically evaluate the quality of the existing canal(s) obturation, identify any missed canals, and assess the extensiveness of a periapical lesion.
Endodontic Retreatment Options
If a previously endodontically treated tooth is restorable and has adequate periradicular cortical and medullary bone, endodontic retreatment can involve either nonsurgical retreatment and/or surgical retreatment. The main determining factors as to which approach a clinician should take are the marginal integrity of the current restoration, the radiographic (CBCT recommended) appearance of the obturation of the canal(s), the morphology of the canal(s), and the periradicular anatomy (ie, proximity of maxillary sinus or inferior alveolar nerve). When assessing a periradicular lesion, the clinician must bear in mind that in forensic endodontics there is no previous clinical or radiographic history to review. The existing lesion could be either growing bigger, becoming smaller, or not changing in size since the original conventional endodontic treatment was performed. Although there is an empirical inclination to endodontically retreat by conventional endodontic treatment, even if the restoration is properly intact and the previous obturation is within normal limits, it is important to understand that if the periradicular lesion is a cyst (requiring biopsy to confirm diagnosis) it may not heal regardless of how well the conventional endodontic treatment or retreatment is performed.9
Surgical retreatment can involve root-end resection/root-end filling technique, root amputation, or intentional replantation.10,11 If a tooth has an extensive fracture (as clinically evident by a deep periodontal probing and radiographic and/or clinical observation) or is nonrestorable, extraction of the tooth and placement of an implant, fixed bridge, or removal appliance is the authors' recommended treatment of choice.
In forensic endodontics the question may arise as to whether or not any treatment should be recommended. This may specifically be the case when a patient presents with an asymptomatic previously endodontically treated tooth with a periapical lesion. No treatment would entail placing the patient on 6-month radiographic recall to monitor if the lesion is getting larger, smaller, or staying the same size. This may be the recommended approach if the endodontic procedure was performed in the past few years; however, forensic endodontics usually involves cases in which teeth had endodontic treatment more than just a few years ago. Therefore, the chance of observing any radiographic change (demonstrating healing) to an existing asymptomatic radiographic lesion at a 6-month recall is negligible.12,13
Forensic Endodontic Case Report: Intentional Replantation
A 55-year-old man was referred by an outside private dentist to the University of Illinois-Chicago College of Dentistry's department of Graduate Endodontics for treatment of tooth No. 18. The patient's chief complaint was "pain to bite on the lower left back tooth," with the patient pointing to tooth No. 18.
The patient's medical and dental histories were reviewed. The medical history was determined to be noncontributory. Blood pressure and pulse were taken and noted to be within normal limits. The patient reported no known drug allergies. His dental history entailed previous restorative treatment.
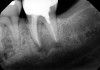
The next step in the diagnostic process was to perform objective clinical sensibility pulpal and periradicular testing to determine the etiology of the patient's chief complaint. A periapical radiograph was taken of tooth No. 18 that showed a radiolucent area present around both the mesial and distal roots(Figure 3). Tooth No. 18 tested abnormal to percussion and bite tests. Palpation, periodontal probings, and mobility were within normal limits. Tooth No. 17 had been previously extracted, and tooth No. 19 tested within normal limits to cold, percussion, palpation, bite test, mobility, and periodontal probing sensibility tests.
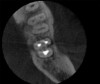
The patient stated that a previous root canal had been performed on tooth No. 18 many years ago, but he had no memory of the exact date or the name of the dentist who provided the treatment. The referring dentist had no records or preoperative radiographs of tooth No. 18 from before the initial endodontic treatment. A limited FOV CBCT scan of the tooth was taken, and a radiolucency was observed on the mesial and distal roots (Figure 4). The pretreatment pulpal diagnosis was "previously treated," and the periradicular diagnosis was symptomatic apical periodontitis.
The clinician determined that the treatment options were conventional endodontic retreatment or endodontic surgery, which would involve resectioning of the mesial and distal roots, preparation of the root ends, and placement of a bioceramic root-end filling. With regard to restorative evaluation, the existing crown on tooth No. 18 was deemed to be within normal limits. Although the periapical radiograph (Figure 3) showed a radiolucent line around the distal portion of the crown, the marginal integrity was determined to be clinically acceptable. The CBCT demonstrated that the inferior alveolar nerve canal was close in proximity to the mesial and distal roots of tooth No. 18. Also, clinically the surgical access around tooth No. 18 was limited for root-end resection endodontic surgery. The axial CBCT view showed that the current canal obturation was within normal limits (Figure 5).
The treatment options for both con--ventional endodontic retreatment and intentional surgical replantation of tooth No. 18, including the pros and cons of each option, were presented to the patient. He was made aware that after a conventional endodontic retreatment there might be a chance that the existing lesion may not heal and further treatment intervention would be required. Also, in the case of performing an intentional replantation, if tooth No. 18 were to have a restoration or root fracture upon extraction, the tooth would not be re-implanted. The patient opted for the intentional replantation since it could be performed in one treatment visit.
A left inferior alveolar nerve block was administered using 68 mg lidocaine with 0.01 mg/ml epinephrine. A long buccal block, along with an intraligamental injection around tooth No. 18, was given with 17 mg Septocaine with 0.01 mg/ml epinephrine. Objective pulpal testing was performed with cold stimulus to confirm the level of pulpal anesthesia as correlated by the lack of patient's subjective response to cold stimulus on tooth No. 19. Also, percussion and bite tests were performed on tooth No. 18 to confirm correlation to the patient's subjective report of profound lower left lip anesthesia. The patient reported no pain to either percussion or bite test on tooth No. 18 after the administration of local anesthesia.
After objective confirmation of profound left mandibular anesthesia, tooth No. 18 was extracted and wrapped in gauze saturated with saline. Under a surgical microscope, the mesial and distal roots were resectioned 3 mm, and the root ends of both the mesial and distal roots were stained with methylene blue and irrigated with saline (Figure 6). Staining was noted around gutta-percha, but no fracture was observed on either root. Root-end ultrasonic preparation was made 3 mm in depth on the mesial and distal roots, and placement of a bioceramic root-end filling was completed.10 The entire root-end preparation and root-end fill was conducted outside the mouth within a 10-minute period.11 Also, during this time the socket of tooth No. 18 was gently curetted to remove granulomatous-type tissue. Not enough tissue could be removed for a biopsy. Tooth No. 18 was then properly reseated in the exposed socket (Figure 7) and sutured into place, and a final periapical radiograph was taken (Figure 8).
The patient was given postoperative instructions and medications (amoxicillin 500 mg, ibuprofen 600 mg, and chlorhexidine mouth rinse). He returned to the clinic 5 days post-treatment for suture removal and evaluation. No radiograph was taken at the 5-day postoperative recall visit. The patient presented with tooth No. 18 intact and slightly mobile and reporting slight discomfort of the surgical area. At a 2-month recall tooth No. 18 was found to be asymptomatic and fully reintegrated into the socket (Figure 9). Mobility and periodontal probings were within normal limits.
Summary
Although forensic endodontics is an empirical concept, it has a clinical application. Forensic endodontics is defined as the determination of the proper pretreatment pulpal and periradicular diagnosis and etiology of a patient's tooth pain and/or periradicular lesion on a tooth that was previously endodontically treated. In forensic endodontics the patient has no recollection of when the tooth in question was treated or by whom. Also, no past records or radiographs are available to the clinician to evaluate the prior endodontic treatment, and therefore a treatment assessment must be made based only on the current presentation of the patient. Endodontic retreatment options in forensic endodontics are conventional nonsurgical retreatment, surgical endodontics, or extraction. An intentional replantation surgical case was presented as a clinical example of performing forensic endodontics.
About the Authors
James Bahcall, DMD, MS
Clinical Professor, Department of Endodontics, University of Illinois-Chicago, College of Dentistry, Chicago, Illinois
Qian Xie, DDS, PhD
Assistant Professor, Department of Endodontics, University of Illinois-Chicago, College of Dentistry, Chicago, Illinois
Mark Baker, DDS
Clinical Associate Professor, Department of Endodontics, University of Illinois-Chicago, College of Dentistry, Chicago, Illinois
Steve Weeks, DDS
Clinical Assistant Professor, Department of Endodontics, University of Illinois-Chicago, College of Dentistry, Chicago, Illinois
Daniel Oh, DDS, MS
Second-year endodontic resident, University of Illinois-Chicago, College of Dentistry, Chicago, Illinois
Queries to the author regarding this course may be submitted to authorqueries@aegiscomm.com.
References
1. Bahcall J, Johnson B. Clinical guide to treating endodontic emergencies. Inside Dentistry. 2016;12(4):46-48.
2. Jain N, Gupta A, Meena N. An insight into neurophysiology of pulpal pain: facts and hypotheses. Korean J Pain. 2013;26(4):347-355.
3. Närhi M, Virtanen A, Kuhta J, Huopaniemi T. Electrical stimulation of teeth with a pulp tester in the cat. Scand J Dent Res. 1979;87(1):32-38.
4. Keir DM, Walker WA 3rd, Schindler WG, Dazey SE. Thermally induced pulpalgia in endodontically treated teeth. J Endod. 1991;17(1):38-40.
5. McCarthy PJ, McClanahan S, Hodges J, Bowles WR. Frequency of localization of the painful tooth by patients presenting for an endodontic emergency. J Endod. 2010;36(5):801-805.
6. AAE Consensus Conference Recommended Diagnostic Terminology. J Endod. 2009;35(12):1634.
7. Uraba S, Ebihara A. Komatsu K, et al. Ability of cone-beam computed tomography to detect periapical lesions that were not detected by periapical radiography: a retrospective assessment according to tooth group. J Endod. 2016;42(8):1186-1190.
8. Patel S, Brown J, Pimentel T, et al. Cone beam computed tomography in endodontics - a review of the literature. Int Endod J. 2019;52(8):1138-1152.
9. Torres-Langares D, Segura-Egea JJ, Rodriguez-Caballero A, et al. Treatment of a large maxillary cyst with marsupialization, decompression, surgical endodontic therapy and enucleation. J Can Dent Assoc. 2011;77:b87.
10. Wang ZH, Zhang MN, Wang J, et al. Outcomes of endodontic microsurgery using a microscope and mineral trioxide aggregate: a prospective cohort study. J Endod. 2017;43(5):694-698.
11. Becker BD. Intentional replantation techniques: a critical review. J Endod. 2018;44(1):14-21.
12. Strange KA, Tawil PZ, Phillips C, et al. Long-term outcomes of endodontic treatment performed with Resilon/Epiphany. J Endod. 2019;45
(5):507-512.
13. Sjögren U, Hägglund B, Sundquist G, Wing K. Factors affecting the long-term results of endodontic treatment. J Endod. 1990;16(10):498-504.