You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
In the course of routine examinations and esthetic evaluations, dentists often encounter patients who present with gingival recession. Defined as exposure of the root surface at the gingival margin, gingival recession is an apical shift in the position of the gingiva secondary to loss of attachment that can negatively affect smile esthetics, increase susceptibility to root caries, and lead to dentin hypersensitivity.1,2 With gingival recession, as the depth and width of recession increases, the amount of periodontal attachment and root coverage decreases.3
Several predisposing conditions may contribute to gingival recession, including a thin alveolar housing, tooth malposition, insufficient supporting alveolar bone, and a deficient amount of attached gingiva, among others.2,4,5 Whether from bacterial plaque or mechanical causes, the etiology of recession is inflammation that ultimately leads to displacement of the soft-tissue margin and root exposure.1,2,5
Therefore, goals in treating gingival recession include: creating an environment that will be more resistant to future recession, covering and increasing the amount of periodontal attachment to previously exposed roots in areas of esthetic concern, increasing the vertical and horizontal dimensions of the barrier periodontium, strengthening the gingival tissue surrounding the tooth, and limiting future recession.6-8 Simultaneously, short-term objectives of treatment focus on minimizing negative consequences to the patient (eg, pain, postoperative healing time), while long-term objectives emphasize achieving stable and predictable outcomes. Complementary goals include improving oral esthetics, decreasing root sensitivity, and increasing an individual's oral hygiene effectiveness on the affected teeth.6-8
Among the viable and effective treatments for remedying gingival recession is root coverage through tissue grafting.9,10 Tissue grafting techniques enable dentists to correct gingival recession by grafting tissues into the area of recession, suturing the graft in place, and allowing it to heal.11-13
Although a variety of grafting techniques have been described over the years, there are essentially three types of grafting therapies for treating gingival recession: pure gingival augmentation with free gingival grafts (FGGs),14 root coverage and gingival augmentation with connective tissue grafts (CTGs),15 and root coverage with acellular dermal matrix (ADM).16 Each therapy is characterized by the type of grafting material used, the manner in which the grafting material is harvested, and the respective technique for placing the grafting material. Understanding the differences among the therapies will benefit dentists when determining the most appropriate treatment for patients who present with gingival recession and areas of deficient attached gingiva.
Pure Gingival Augmentation With Free Gingival Grafts
Pure gingival augmentation with FGGs usually does not involve significant coverage of the roots.11,14 Instead, FGGs aim to increase the strength of the soft tissue for resistance against future recession by increasing not only the vertical dimension of the gingiva, but more importantly, its horizontal thickness. This procedure is technically less difficult to perform than a CTG or an ADM graft.11,14
A limitation, however, is that a FGG does not resemble adjacent tissues, which may present esthetic shortcomings.17 The FGG is taken from the palate and includes the epithelial layer and some connective tissue below the epithelium (ie, a combination of epithelium on the outer layer and a connective tissue layer below).
To procure a FGG, the tissue to be harvested is outlined using a #15C scalpel, then any rugae on the graft are smoothed off with a coarse #10 round diamond bur before removal of the graft (Figure 1). Smoothing the rugae reduces its appearance on the graft postoperatively for esthetic purposes and ensures equal thickness of the graft while it is being removed from the palate. Typically, a FGG is 1.5 mm to 2 mm thick. However, if more thickness is needed to try to gain root coverage, 2 mm to 2.5 mm can be harvested.18
The graft is undermined by making an incision into the connective tissue layer using a #15C scalpel, leaving the epithelial layer intact (Figure 2). The tissue can then be lifted away and freed from the palate (Figure 3), after which it can be trimmed as necessary and ultimately transplanted back to the patient. The palate is then covered with a positive-pressure stent worn by the patient continuously for 1 week postoperatively, except when cleaning the stent after eating. During the second week postoperatively, the patient wears the stent only when eating. The palate is expected to be fully healed after the second week and then no longer requires protection. Surgical dressing is placed on the graft recipient site to reduce postoperative discomfort and facilitate proper healing of the graft site.
Typical FGG Case
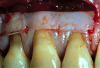
A male patient in his 30s presented for treatment of increasing recession he had had over his lifetime. Upon examination, a complete lack of gingiva on the facial of tooth No. 6 was observed. Although he had about 1.5 mm of gingiva on the facial of tooth No. 7 (Figure 4), both teeth probed to 3 mm. This indicated an absence of attached gingiva on the facial of these teeth in addition to increasing recession.
With a low lip line, the patient was not concerned about esthetics, and he was not experiencing root sensitivity. It was determined and agreed that a FGG was the best option for him in order to increase the amount of gingiva and limit further recession.
The graft was placed to the height of the original free gingival margin (FGM) (Figure 5), and no attempt was made to cover what had been the exposed root areas—the only areas covered were where biologic attachment had been previously. Interproximal sutures were used to hold the FGG in place, and a surgical dressing was applied. Figure 6 shows successful 13-year results.
Note that when FGGs fit passively onto the recipient site with complete contact on the underlining recipient bed, apical sutures are not required. However, when grafts tend to lift off the recipient site, from which the grafts obtain their blood supply, apical sutures are necessary to maintain intimate contact and fit.11,14,17
Considerations for Advanced FGG Cases
There are times when two separate grafts must be taken and sutured together to create a single long graft capable of treating several adjacent teeth simultaneously. A split-thickness recipient site eliminating the prior FGM, gingiva, and mucosa at the site is used for grafting; this is known as a “marginal” graft. The grafts are stabilized with sutures placed between the affected teeth in the base of the papillae, the mesial and distal apical corners, as well as in the apical area when necessary to prevent lifting from the recipient site. For the long term, these grafts provide better esthetics than a “submarginal” graft by eliminating the transition zone between thin and thick tissue at the FGM.11,14,17,19,20
Over time, such large FGGs placed at the FGM tend to experience “creeping reattachment,” a phenomenon in which the graft creeps coronally on the root, increasing the amount of root coverage. This likely occurs as a result of circumferential fibers reestablishing themselves through the graft after surgery, tightening and shifting coronally around the teeth over time.20
Additionally, in some cases FGGs may be necessary for root coverage, such as situations where friable, thin, and fragile tissue exists that is not suitable for CTGs or ADM grafts.19 In such instances, thick gingival grafts of about 2 mm to 2.5 mm thickness may be taken from the palate (ie, epithelial layer and the underlying connective tissue) and placed over the roots of the teeth. To maintain a very intimate contact between the graft and underlying recipient site, sutures are placed between every tooth.
Root Coverage With Connective Tissue Grafts
CTGs, which are taken from deeper in the palate than a FGG—from under the epithelium—can increase the vertical and horizontal dimensions of the attached gingiva, similar to FGGs.12,15 However, CTGs also enable predictable coverage and attachment to previously exposed root areas, procedures that are less predictable with FGGs.12,15 CTGs not only limit future recession, but also improve esthetics and increase attachment to the tooth, making this a highly versatile grafting option.12,21
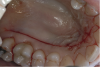
Harvesting a CTG requires displacing the epithelial layer to access the connective tissue.22 This can be accomplished with the creation of a “trap door” on the palate, which is made with a single horizontal incision. If more release is required, the incision is continued around the arch of the palate to the other side (Figure 7). The “trap door” consists of the outer epithelial layer and a thin layer of connective tissue; some connective tissue should remain on the flap to prevent sloughing during the healing process.15,21,22
Such an approach, which also leaves the periosteum of the palate intact, enables harvesting of ample connective tissue but also facilitates rapid donor site healing. The flap is lifted with a #15C scalpel (Figure 8), and the connective tissue is removed. Typically about 1.5 mm to 2 mm of tissue thickness and 4 mm to 6 mm of tissue width, by whatever length is necessary to cover the number of teeth involved, is harvested.22
After the connective tissue has been harvested, the palatal flap is sutured using 6-0 resorbable suture with a half-round, small needle, which enables easy in-and-out suturing without looping around the teeth. In particular, the suture is tied on the distal, run forward as a continuous suture, and then tied off at the mesial. As with the FGG procedure a positive-pressure palatal stent is used postoperatively.
Among the techniques for placing CTGs are the tunnel flap technique and envelope approach.19,23-26 With the tunnel flap technique, all graft placement surgery is completed through the sulcus.15,23 The envelope approach involves a flap created with incisions at the base of each papilla as well as the sulcus.25 With either flap design, leaving some of the CTG partially exposed will stimulate growth of more epithelialized tissue through migration from the wound margins over the exposed connective tissue, thereby creating more gingiva.15,19,24,27,28
Typical CTG Case—Envelope Technique
A patient presented with moderate recession requiring root coverage and increased thickness of the alveolar housing (Figure 9). A series of parallel incisions was completed using instruments made specifically for microsurgery; these incisions were performed utilizing high magnification (ie, 5.5 magnification via loupes). The distance between the incisions was roughly the amount of root coverage necessary on the adjacent teeth (Figure 10).25
The isthmus of tissue between the parallel incisions was removed. A split-thickness flap was elevated leaving connective tissue on the bone and providing access for root preparation.
To ensure a smooth root surface, rotary instruments with finishing burs and curettes are used. A glycine air-polishing unit (eg, Air-Flow Master, Hu-Friedy, hu-friedy.com) was used to impart the final smoothing of the roots and remove the smear layer and biofilm.
The CTG was then harvested from the palate as previously described and placed over the roots (Figure 11). The primary flap was advanced to cover the graft; a dual blood supply was assured from the underlying tissue and the overlying flap. Atraumatic suturing was performed using fine sutures (eg, Resorba® 6-0/7-0 Resolon™, Osteogenics Biomedical, osteogenics.com) to approximate the flap margins.
After 1 week, rapid healing and good closure were observed. After 2 years, complete root coverage was visible, a thicker alveolar housing was achieved, and the gingiva was more resistant to future breakdown (Figure 12).
Root Coverage With Acellular Dermal Matrix
An ADM graft does not involve a patient donor site. Rather, typically it is donated human dermis processed at a skin bank to remove the epidermis and cells, and then it is freeze-dried. Ultimately, the ADM is forwarded to the dentist for use in gingival grafting procedures.
The purpose and goals for utilizing ADM are the same as for using CTGs. Although all cases indicated for root coverage and gingival augmentation can be treated with CTGs, only a subset can be successfully treated with ADM with greater ease for both the patient and surgeon while simultaneously avoiding the palate.10,13,16 The author finds that in approximately half of the cases in his office requiring soft-tissue grafting ADM is appropriate therapy.
Based on clinical outcomes, the author recommends that ADM is indicated when gingival recession is present and at least 1.5 mm of gingiva remains. ADM cannot be used to increase the amount of gingiva, and mucosal margins can be problematic around teeth. When there is a total deficiency of gingiva, FGGs or CTGs are preferred as they can be manipulated surgically to increase the amount of gingiva.10,13,16
Typical ADM Case
A female patient presented with composite restorations along the gingival margins that had been placed in an attempt to correct the appearance of gingival recession (Figure 13). The extent of the recession was visible in her smile, and the patient desired improved esthetics.
The composite restorations were removed in anticipation of covering the roots with ADM; this, however, exposed a deficiency in the underlying enamel. The patient and restorative dentist planned the position of a new cementoenamel junction (CEJ) using restorative material. This was accomplished using a glass-ionomer material—which bonds to dentin—on the dentin surfaces covered by a veneer of composite that would polish easily, provide a more esthetic appearance, and bond to the enamel at the coronal aspect of the restoration. This bilayer approach also would prevent marginal leakage around the restorations.
Once the “new” CEJ was established, a tunnel flap was created to enable placement of the ADM through the sulcus. The attachment to the tooth and underlying bone was dissected using a series of precision micro-instruments (eg, Allen Oral Plastic Surgery Kit, Hu-Friedy) designed for oral plastic surgery. The papillae were also loosened from the facial to the palate. This provided ample working room and access with minimal trauma to the patient and minimal postoperative complications or discomfort.26
Once elevated, the flaps were displaced laterally and held out of the way while finishing burs and hand instruments were used to reshape and smooth the tooth roots (Figure 14). The roots were then cleansed with glycine air polishing.
The selected ADM was rehydrated with saline and, in this case, a platelet-derived growth factor (PDGF) (eg, Gem 21S®, Osteohealth, osteohealth.com) was added onto it prior to placement. PDGF, which is a mitogenic and angiogenic material shown to speed soft-tissue healing and promote cell attachment to the roots, may also be used during advanced cases of connective tissue grafting.29
The ADM was introduced into the sulcus, and the graft was advanced laterally to cover all of the affected teeth. The ADM was positioned under the tissue and sutured to ensure stability of the FGM and secure the fibrin clot (Figure 15).
After 2 years, the FGM position was maintained in a coronal position relative to where it had been preoperatively (Figure 16). Stable root coverage was achieved, along with an esthetic enhancement to the patient's smile.
Conclusion
Treating areas of deficient attached gingiva and recession with autogenous tissue grafting (eg, free gingival grafts or connective tissue grafts) or acellular dermal matrix presents several advantages. The gingival tissues surrounding the teeth are strengthened to resist further recession; therefore, root surfaces are less likely to become increasingly exposed over time. When root surfaces are covered, the roots are no longer exposed to potential pathogenic plaque or erosive agents. Sensitivity may be reduced, and the esthetics of the gingival architecture is enhanced. Depending upon the specific needs of the case, pure gingival augmentation with free gingival grafts, root coverage with connective tissue grafts, or root coverage with acellular dermal matrix can be effective ways to treat gingival recession and areas of deficient attached gingiva.
ABOUT THE AUTHOR
Kirk Pasquinelli, DDS
Private Practice limited to periodontics, bone augmentation, and dental implants, San Francisco, California; Assistant Clinical Professor, Division of Graduate Prosthodontics, University of California at San Francisco School of Dentistry, San Francisco, California
Queries to the author regarding this course may be submitted to authorqueries@aegiscomm.com.
References
1. The American Academy of Periodontology. Glossary of Periodontal Terms. 4th ed. Chicago, IL: American Academy of Periodontology; 2001.
2. Kassab MM, Cohen RE. The etiology and prevalence of gingival recession. J Am Dent Assoc.2003;134(2):220-225.
3. Allen AL. Use of the supraperiosteal envelope in soft tissue grafting for root coverage. II. Clinical results. Int J Periodontics Restorative Dent. 1994;14(4):302-315.
4. Slutzkey S, Levin L. Gingival recession in young adults: occurrence, severity, and relationship to past orthodontic treatment and oral piercing. Am J Orthod Dentofacial Orthop. 2008;134(5):652-656.
5. Ustun K, Sari Z, Orucoglu H, et al. Severe gingival recession caused by traumatic occlusion and mucogingival stress: a case report. Eur J Dent. 2008;2(2):127-133.
6. Wennstrom JL. Mucogingival therapy. Ann Periodontol. 1996;1(1):671-701.
7. Kassab MM, Badawi H, Dentino AR. Treatment of gingival recession. Dent Clin North Am. 2010;54(1):129-140.
8. Bouchard P, Malet J, Borghetti A. Decision-making in aesthetics: root coverage revisited. Periodontol 2000. 2001;27:97-120.
9. Saha S, Bateman GJ. Mucogingival grafting procedures—an update. Dent Update.2008;35(8):561-568.
10. Zuhr O, Bäumer D, Hürzeler M. The addition of soft tissue replacement grafts in plastic periodontal and implant surgery: critical elements in design and execution. J Clin Periodontol. 2014;41 suppl 15;S123-S142.
11. Matter J. Free gingival grafts for the treatment of gingival recession. A review of some techniques. J Clin Periodontal. 1982;9(2):103-114.
12. Wessel JR, Tatakis DN. Patient outcomes following subepithelial connective tissue graft and free gingival graft procedures. J Periodontol. 2008;79(3):425-430.
13. Clozza E, Suzuki T, Engebretson SP. Full-mouth esthetic rehabilitation with acellular dermal matrix. Int J Esthet Dent. 2014;9(4):468-479.
14. Scheyer ET, Sanz M, Dibart S, et al. Periodontal soft tissue non-root coverage procedures: a consensus report from the AAP Regeneration Workshop. J Periodontol. 2015;86(2 suppl):S73-S76.
15. Al-Zahrani MS, Bissada NF. Predictability of connective tissue grafts for root coverage: clinical perspectives and a review of the literature. Quintessence Int. 2005;36(9):609-616.
16. Agarwal C, Tarun Kumar AB, Mehta DS. Comparative evaluation of free gingival graft and AlloDerm® in enhancing the width of attached gingival: A clinical study. Contemp Clin Dent. 2015;6(4):483-488.
17. Patel M, Nixon PJ, Chan MF. Gingival recession: part 3. Surgical management using free grafts and guided tissue regeneration. Br Dent J. 2011;211(8):353-358.
18. Miller PD Jr. Root coverage using a free soft tissue autograft following citric acid application. Part 1: Technique. Int J Periodontics Restorative Dent. 1982;2(1):65-70.
19. Vergara JA, Caffesse RG. Localized gingival recessions treated with the original envelope technique: a report of 50 consecutive patients. J Periodontol. 2004;75(10):1397-1403.
20. Agudio G, Chambrone L, Pini Prato G. Biologic remodeling of periodontal dimensions of areas treated with gingival augmentation procedure: a 25-year follow-up observation. J Periodontol. 2017;88(7):634-642.
21. Langer B, Langer L. Subepithelial connective tissue graft technique for root coverage. J Periodontol. 1985;56(12):715-720.
22. McLeod DE, Reyes E, Branch-Mays G. Treatment of multiple areas of gingival recession using a simple harvesting technique for autogenous connective tissue graft. J Periodontol.2009;80(10):1680-1687.
23. Khuller N. Coverage of gingival recession using tunnel connective tissue graft technique. J Indian Soc Periodontol.2009;13(2):101-105.
24. Abundo R, Corrente G, des Ambrois AB, et al. A connective tissue graft envelope technique for the treatment of single gingival recessions: a 1-year study. Int J Periodontics Restorative Dent. 2009;29(6):593-597.
25. Shanelec DA. Periodontal microsurgery. J Esthet Restor Dent. 2003:15(7):402-407.
26. Allen AL. Use of the supraperiosteal envelope in soft tissue grafting for root coverage. I. Rationale and technique. Int J Periodontics Restorative Dent. 1994;14(3):216-227.
27. Park JB. A two-stage approach using an autogenous masticatory mucosal graft and an autogenous connective tissue graft to treat gingival recession: a case report. J Int Acad Periodontol.2010;12(2):45-48.
28. Harris RJ, Harris LE, Harris CR, Harris AJ. Evaluation of root coverage with connective tissue grafts obtained from the same location. Int J Periodontics Restorative Dent. 2007;27(4):333-339.
29. Lynch SE, Wisner-Lynch L, Nevins M, Nevins ML. A new era in periodontal and periimplant regeneration: use of growth-factor enhanced matrices incorporating rhPDGF. Compend Contin Educ Dent. 2006;27(12):672-678.