You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
The goals of clinical restorative dentistry have been carefully scrutinized by both patients and dentists for many years. Preservation of demineralized non-cavitated enamel and/or dentin1 and stabilization or gain of the periodontal attachment apparatus2 are considered to be the hallmarks of minimally invasive dentistry. At the same time, restorations need to be accurate, precise, durable, and biologically compatible with human tissues. Most dentists learn these goals as part of their fundamental training in dental school. Today, dental students and practicing dentists are required to inform patients of the options available for replacing a single posterior molar, ie, either do nothing, place a fixed bridge, or place a single-tooth implant.
Despite the success of single-tooth implants, dentists have continued to use the fixed partial denture for the primary replacement of a missing posterior molar. This approach may necessitate significant loss of non-diseased tooth structure on abutment teeth; therefore, in many cases the single-tooth implant becomes the treatment of choice.3 The use of a single-tooth implant with either a cement- or screw-retained crown to replace a missing posterior tooth is a highly conservative alternative for patients.4
Conventional crown-and-bridge techniques have been supported by the use of elastomeric impression materials. These impressions require the use of gypsum poured dental models in the laboratory to fabricate the prosthesis. Inherent errors can be introduced in this workflow that may compromise the fit of the final prosthesis. All elastomeric impression materials for dental prosthodontics exhibit some degree of dimensional change during setting.5 For patients who require dental impressions with elastomeric materials, the experience can be stressful, full of anxiety, and less than desirable.
In an attempt to improve restorative procedures, Mörmann et al were the first to utilize computer-assisted design/computer-assisted manufacturing (CAD/CAM) technology for dental inlays and onlays in 1987.6 Although limited in its scope, the technology was the tipping point for the start of digital dentistry. In the mid-1990s the Procera® AllCeram core (Nobel Biocare, nobelbiocare.com) was released; it was the first CAD substructure of 99.9% alumina that allowed veneering of feldspathic porcelain to complete the crown.6 Today, numerous dental companies offer digital solutions in scanning, designing, and milling of many biomaterials for the purpose of providing same-day final restorations or delayed insertion restorations.7
Dental companies are innovating quickly to provide clinicians and laboratories with products and services that provide all-digital solutions for patients. Harvard Business School Professor, Clayton Christensen, has described the concept of disruptive innovation as a process by which a product or service takes root initially in simple applications, at the bottom of a market. The first iterations provide simple, accessible, and basic services, but then the products relentlessly move up market, eventually displacing established competitors. He states that if industries tend to innovate faster than the customers evolve, then eventually they'll produce products or services that are actually too sophisticated, too expensive, and too complicated for many customers in their market.8
The purpose of this article is to provide clinicians with an understanding of the changing landscape that the disruptive innovation of all-digital dentistry is creating in oral health-care with specific focus on oral implantology. Clinicians need to weigh the pros and cons of traditional versus digital workflows. With the advent of evidence-based dentistry, it is important to search for systematic reviews with meta-analysis, understand the clinician's experience level, and be cognizant of patient feedback on digital dentistry. A clinical case report will present an all-digital solution to replace a single posterior edentulous space using a scan-only software with an intraoral scanner that utilizes an open system. A workflow will also be described that provides patients with a restorative solution that can be generated faster and that is more effective than traditional implant surgery and prosthodontics.
State-of-the-Art CAD/CAM Systems
A totally digital workflow starts with the data capture in the dental office. An intraoral scan device captures the necessary intraoral features, creating a digital impression of the prosthetic worksite. The digital image capture may be of a prepared tooth or of an implant scan body attached to the head of an implant. The dental implant may have been placed in the past and undergone osseointegration, or it may have been immediately placed in a newly created socket.
The file generated from an intraoral scan is a Standard Tessellation Language, or STL, file. Scan bodies provided by matching implant vendors or third-party companies are attached to the implant being scanned (Figure 1). After scanning of the scan body, emergence profile of the healing abutment, and the opposing arch, the STL file can be sent via CAD software for the design and milling of a restoration. An open STL file can be sent to most dental laboratories and then imported into design software from many vendors. Common software products for designing dental implant prosthodontics include NobelClinician® or NobelDesign® (Nobel Biocare), Abutment Designer (3Shape, 3shape.com), and Straumann® CARES® X-Stream™ (Straumann, straumann.us).
The design software enables the technician to open a STL file and design implant prosthetic components, ie, custom abutments and cement- and screw-retained crowns. Additional applications for open STL files include orthodontic aligners, occlusal guards, surgical guides, digital articulation, and digitally printed models. The laboratory technician can elect to use an all-digital workflow or a partially digital workflow with the fabrication of a 3-dimensional (3D)-printed stereolithographic model. Examples of commercially available open architecture STL systems are iTero® (Align Technology, itero.com), True Definition (3M ESPE, 3m.com), PlanScan® (Planmeca CAD/CAM, planmecausa.com), CS 3500 (Carestream Dental, carestreamdental.com), TRIOS® (3Shape), and Aadva™ IOS (GC America, gcamerica.com).
Some manufacturers have elected to design a closed system protocol that allows the STL file to be imported only into their proprietary software for design and milling. Well-known in digital dentistry, the CEREC® system, CEREC AC Omnicam (Dentsply Sirona, sirona.com), uses a closed system for design and milling of traditional crowns or implant prosthodontics. In most cases a dentist using CEREC technology will design and mill the final crown in the office for an all-digital workflow.
Regardless of whether the practice selects an open or closed STL system, the dentist and staff will need to undergo thorough training to learn the use of commercially available software and hardware. The training should be specific to the applications available with their scanner, milling, and fabrication options. Though training in all aspects of prosthetic design and manufacturing is encouraged, some dentists may only receive scanning training because the design and milling will be outsourced to a commercial laboratory that utilizes its specialized software. If an all-digital/all-in-office closed system, ie, CEREC, is used, the dental team will also need to be trained in the design and milling that is also done in the office.
If in-office milling is elected for “same-day” dentistry, then additional in-office devices and procedures will be necessary for delivery of the final restoration. Additional chairtime will be required for designing and milling the crown, sintering, glazing and staining if needed, polishing, and, finally, seating and adjusting the crown in the mouth prior to cementation. It may take between 1 to 2 hours to complete an in-office same-day all-digital solution depending on the clinician's training and skill level.
Additional upfront costs for this protocol include an in-office mill, design software, dust extractor, upgraded dental compressor, dental furnace, and CAD/CAM polyceramic monolithic blocks (including a complete inventory of all shades in the shade guide) for milling. Different materials require more or less milling time in the in-office milling device, depending on the material chosen for the patient. In some cases, long-term provisional restorations or custom healing abutments may be milled out of polymethyl methacrylate (PMMA) blocks. With the advent of affordable desktop 3D printers, some dentists are fabricating models or implant surgical guides in the office for diagnosis and implant surgical placement with fully or partially guided drilling protocols.
The clinician should carefully consider several factors when determining whether to purchase an open or closed system. The decision should be based on practice objectives, patient preferences, and the economics, ie, return on investment, associated with any digital dentistry system. Both systems will affect fixed overhead and variable overhead. Whichever system is preferred, it can be financed, leased, or purchased outright, and consultation with a financial advisor can be helpful in this regard. In addition to the initial costs of obtaining hardware, software, and materials, other costs will include recurring usage fees, software upgrades, warranties, and occasional training expenses. The support staffs, including office managers, administrative assistants, hygienists, and dental assistants, will need to grasp new scheduling requirements, fees, and technique to adapt to the purchased system. Clinicians will need to set appropriate training schedules with vendors to ensure the staff is properly trained in digital dentistry protocols. Some referral-basis practitioners, periodontists, and oral surgeons can provide scanning services for restorative dentists that may dramatically increase the dentist's profitability.
If dentists elect to only perform intraoral scans, whether with a closed or open system, they also must partner with laboratories to provide the outsourced procedures of design and milling. Laboratories, in turn, must decide if they want to design and mill or design only and then have a third-party milling center complete the restoration off site. Significant investments in hardware and software training are required in the lab to operate design software and milling devices, and outsourcing milling to a specialized laboratory may help to defray costs. Because all of the data obtained by intraoral or benchtop scanners can be transferred via HIPAA-secure STL files, in many cases the laboratory becomes an assembler of all the components required to complete an implant restorative procedure.
One aspect of digital dentistry that is frequently overlooked is the ability of the clinician to participate in digitized interdisciplinary care. Most software packages used in open systems allow sharing of planning and design via the Internet from proprietary “clouds” set up by providers of digital solutions. These HIPAA-compliant sharing modules help the clinicians, surgeons, laboratory technicians, and patients better understand upfront the diagnosis, risks/benefits, costs, and informed consents necessary to perform interdisciplinary care. Documents, files, and viewers are cloud-based, allowing the dental team to access them from anywhere in the world. Dental management software can be linked with these new systems to provide a paperless solution. All-digital solutions also offer a “green” effect as data is distributed via the Internet, reducing the need for carbon-based transportation involved in the manufacturing and delivery of the prosthesis.
Finally, due to the absence of physical models and reduced manpower requirements compared with traditional gypsum-based protocols, some dental laboratories offer lowered fees for digitally submitted cases. Because the intraoral scanner converts the image to a digital STL file, the lab can immediately start the design process without needing to pour models, allow setting, perform articulation, and scan with a desktop scanner. This can lower overall overhead and ultimately the variable costs associated with fabrication of the implant prosthesis. Typically, digital dentistry open systems enable the lab to decrease in-lab case time, and some prosthetic components may be returned to the submitting clinician the same or next day.
Intraoral Scanning CAD/CAM Dentistry: Literature Review
Because of the exacting nature of implant prosthodontics, implant dentistry has enjoyed a high degree of precision due to the quality of machining implant bodies and abutments via CAD/CAM.9 In their systematic review of CAD/CAM technology, Kapos and Evans suggested that a new definition be applied to a restoration where no or minimal manual intervention is used: “complete CAD/CAM product.”9 Long-term success of implant prosthetics includes matched implant system components, a precise fit, connection between the abutment and implant, and appropriate preload.10 It is incumbent on clinicians to use implant components from one manufacturer only and not assume that other brands are compatible, interchangeable, or capable of reproducing intimate fits that screw-retained restorations require.11 An intimate and passive fit with proper preload is necessary in screw-retained crowns for long-term integrity of the prosthesis and optimal performance.
Lee et al compared the accuracy of 30 sets of gypsum models acquired from conventional implant impressions to digitally milled models created from direct digitalization by 3D analysis. They found that milled models from digital impressions were comparable to gypsum models from conventional impressions.12 A systematic review by Chochlidakis et al of digital impressions versus conventional impressions for fixed prostheses concluded that digital impressions provided better margins and internal fit of restorations than did conventional techniques.13
Vandeweghe et al evaluated various intraoral scanning devices in an in vitro study of scanning six external hex implants with polyether ether ketone (PEEK) scan bodies. The authors noted that the digital scanners with the highest degree of accuracy were the 3M True Definition, an open platform system that employs a blue light-emitting diode (LED) light and a video imaging system with a light dusting of titanium-oxide powder, and the TRIOS, a powderless open file system based on confocal microscopy.14 An American Dental Association Professional Product Review study by Hack and Patzelt in 2015 evaluated the accuracy of six intraoral scanning devices.15 The analysis found the highest precision values for accuracy in scanning a single molar abutment tooth in vitro were for TRIOS (4.5 ± 0.9 µm), True Definition (6.1 ± 1.0 μm), iTero (7.0 ± 1.4 μm), and CS 3500 (7.2 ± 1.7 μm).
Economic Considerations
In light of post-recession economic conditions that have persisted in the United States, dentists are attempting to make their practices more efficient.16According to the American Dental Association (ADA), general dentists' gross billing per practice hour averages US $404.17 Traditional protocols for implant prosthodontics that require the use of mixing machines/garant guns, adhesives, trays, mixing tips, bite registration/facebow materials, and implant impression analogs can be eliminated with digital methods. However, upfront costs of acquiring an intraoral scanner, scan bodies, and training for an all-digital in-office scan-only approach typically range between $15,000 and $35,000. If digital impression systems are used with a scan-only digital workflow in the dental office with design and milling being outsourced, the variable costs of an all-digital solution—including milling blocks, diamond burs, distilled water/powders, and machine maintenance—are paid by the dental laboratory. In turn, the laboratory back-charges the dentist for these services and the manufactured prosthetic components.
Lee and Gallucci evaluated the time efficiency of intraoral scanning; specifically, they assessed the efficiency of digital and conventional impressions of single-implant restoration models taken by second-year dental students. The mean total treatment time (preparation time plus working time including retakes/rescans) was 24 minutes 42 seconds for the conventional approach and 12 minutes 29 seconds for the digital approach, with a statistically significant difference of more than 12 minutes (P < .001).18 A study by Patzelt et al found that use of intraoral scanners for computer-aided impression making was significantly faster than conventional impressions.19
Because the intraoral image capture significantly decreases chairtime for a single-tooth solution, the net effect on fixed and variable expenses can be significant. ADA data suggests most dentists achieve an hourly goal of $404 per hour or $6.73 per minute.17 Based on the Lee and Galluci study cited above,18 the 12 minutes in time saved multiplied by $6.73 would yield $80.76 in increased production time. If, for example, a dentist places an average of 500 crowns per year, including crowns on both implants and naturally prepared teeth, multiplying this number by $80.76 would result in $40,380 in increased production for the year. Furthermore, in actual practice some might consider the 12 minutes in time savings per treatment a conservative estimate.
Additional time efficiencies can be achieved by developing a digital impression workflow that allows the dentists and assistants to share responsibility of opposing arch scans, area scans, and scan-body captures. Experienced users of digital technology feel that the process is more time efficient and preferred by staff and report that patient feedback is excellent.20
Case Presentation
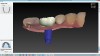
A mandibular right first molar was extracted due to an advanced Class III furcation and an irreversible pulpitis—a combination lesion. An immediate implant placement protocol was elected, and a PEEK abutment was placed on the implant (Figure 1). After 3 months of healing, a scan body was placed on the osseointegrated implant (Figure 2 and Figure 3), and an intraoral scan was taken (TRIOS Pod) (Figure 4) for the fabrication of a screw-retained crown.
Once the STL file generated from the intraoral scanner was sent to the laboratory (Figure 5), the technician used proprietary software to design the crown (Figure 6 through Figure 8), mill the crown, and digitally print a SLA model (Dental SG, Formlabs, www.formlabs.com) (Figure 9 through Figure 11), and then finish the crown on the digitally printed model. The angulated screw-channel full-zirconia crown (Nobel Biocare) (Figure 12) was seated, and contacts were evaluated intraorally and adjusted extraorally. The screw-retained crown was torqued to 35 Ncm2, and the screw access was sealed (Figure 13 through Figure 15).
After the access hole was sealed, an articulating media was used to provide adequate occlusal and/or axial anatomy for functional purposes. Finishing kits should be used with air-stream and water to cool the zirconia so as to not disturb the zirconia crystalline structure. Intraorally, final finishing with a rubber cup and a polishing paste can increase surface smoothness and durability of the zirconia crown.
Summary
The use of CAD/CAM technology for the design and manufacture of dental prostheses is supplanting conventional workflows in the laboratory setting due to time efficiencies and operator preference.21 Implant dentistry has been a primary beneficiary of the digital revolution. High-quality implant fixtures and abutments for implant prosthetics favorably impact peri-implant health. Due to proprietary rights, it is difficult to compare various implants from different manufacturers and the long-term outcomes of implant prosthetics. However, it appears that CAD/CAM-produced products can match the success of conventionally fabricated components.
A central concept to intraoral scanning in the dental operatory is the provision of quicker input for the prosthesis workflow without the use of conventional dental processes and materials. By capturing the data via an intraoral device, the workflow can start immediately in the dental laboratory once the STL file is sent via a HIPAA-compliant Internet connection. If a “complete CAD/CAM product” is desired, then design, milling, and production of a prosthesis can take place within a couple of minutes. The rapidity with which restorations can be manufactured has a bearing on the patient experience in implant dentistry. By achieving “sooner to teeth solutions” the interdisciplinary team can reduce the time the patient experiences an edentulous site while providing predictable outcomes.
Consumer demand for conservative prosthetics to replace missing teeth is likely to increase the interest of dentists to offer this state-of-the-art service. A dentist may also design, digitally print, and mill prostheses in-office or outsource these procedures to a third-party laboratory. Referral-based dental practices may incorporate intraoral workflows into their practice to enhance the patient's experience and provide economic benefits to the patient, referral source, and dental laboratory.
Because of the evolving nature of disruptive innovations, it is important that clinicians and laboratory technicians constantly obtain continuing education regarding software and hardware upgrades in digital dentistry. Online support for training and upgrades will be a key component for practices implementing this technology. Advances and generational shifts in CAD/CAM processes will continue to occur as new technologies come to market. Dentists will need to understand the economic investments necessary to obtain this technology and how it will affect the fixed and variable expenses in their clinical practice. Based on recent advances and offerings in intraoral scanning, these technologies may potentially become part of the standardized workflow in clinical practice required to produce high survival rates for implant-supported prosthetics.
ABOUT THE AUTHOR
George V. Duello, DDS, MS
Private Practice, Periodontology and Implantology, St. Louis, Missouri; Fellow, Academy of General Dentistry
Queries to the author regarding this course may be submitted to
authorqueries@aegiscomm.com.
References
1. Murdoch-Kinch CA, McLean ME. Minimally invasive dentistry. J Am Dent Assoc. 2003;134(1):87-95.
2. Parameter on chronic periodontitis with slight to moderate loss of periodontal support. American Academy of Periodontology. J Periodont. 2000;71(5 suppl):853-855.
3. Christensen GJ. Three-unit fixed prostheses versus implant-supported single crowns. J Am Dent Assoc. 2008;139(2):191-194.
4. Farran H. Dentists are still doing way too many three-unit bridges. Dentaltown. August 2013:12-16.
5. Burgess JO. Impression material basics. Inside Dentistry. 2005;1(1):30-33.
6. Mörmann WH, Brandestini M, Lutz F. The Cerec system: computer-assisted preparation of direct ceramic inlays in 1 setting [in German]. Quintessenz. 1987;38(3):457-470.
7. Duplantis CC. The current state of digital impression systems in dentistry. Inside Dentistry. 2006;2(8):48-54.
8. Christensen CM. The Innovator's Dilemma: When New Technologies Cause Great Firms to Fail. Boston, MA: Harvard Business Review Press; 1997:231-237.
9. Kapos T, Evans C. CAD/CAM technology for implant abutments, crowns, and superstructures. Int J Oral Maxillofac Implants.2014;29(suppl):117-136.
10. Hurson S. Use of authentic, integrated dental implant components vital to predictability and successful long-term clinical outcomes. Compend Contin Educ Dent.2016;37(7):450-455.
11. Zanardi PR, Costa B, Stegun RC, et al. Connecting accuracy of interchanged prosthetic abutments to different dental implants using scanning electron microscopy. Braz Dent J. 2012;23(5):502-507.
12. Lee SJ, Betensky RA, Gianneschi GE, Gallucci GO. Accuracy of digital versus conventional implant impressions. Clin Oral Implant Res. 2015:26(6):715-719.
13. Chochlidakis KM, Papaspyridakos P, Geminiani A, et al. Digital versus conventional impressions for fixed prosthodontics: A systematic review and meta-analysis. J Prosthet Dent. 2016;116(2):184-190.
14. Vandeweghe S, Vervack V, Dierens M, De Bruyn H. Accuracy of digital impressions of multiple dental implants: an in vitro study. Clin Oral Implants Res. 2017;28(6):648-653.
15. Hack GD, Patzelt SB. Evaluation of the accuracy of six intraoral scanning devices: an in-vitro investigation. ADA Professional Product Review. 2015;10(4):1-5.
16. Glassman P. Disruptive innovation and the oral health system. J Am Coll Dent. 2016;83(2):4-13.
17. Health Policy Institute, American Dental Association, J Am Dent Assoc. Table 9: Gross Billings Per Hour, Per Visit for Solo Dentists in Private Practice, 2014.
18. Lee SJ, Gallucci GO. Digital vs. conventional implant impressions: efficiency outcomes. Clin Oral Implants Res. 2013;24(1):111-115.
19. Patzelt SB, Lamprinos C, Stampf S, Att W. The time efficiency of intraoral scanners: an in vitro comparative study. J Am Dent Assoc. 2014;
145(6):542-551.
20. Mitchem C. Why digital impressions? Dental Economics. 2012;102(1):32,54,88.
21. Joda T, Lenherr P, Dedem P, et al. Time efficiency, difficulty, and operator's preference comparing digital and conventional implant impressions: a randomized controlled trial. Clin Oral Implants Res. 2017;28(10):1318-1323.