You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
The evolution of implant dentistry has brought improvements in techniques and designs aimed at enhancing implant osseointegration while avoiding potential complications. However, even with such advances, problems can and still do occur.1 Most of the literature on prosthetic complications has focused on screw loosening, screw fractures, abutment loosening, abutment fractures, implant fractures, opposing prosthesis fractures, framework resin/veneering material fractures, implant prosthesis fractures, loss of retention, and overdenture mechanical retention problems.1-3
Higher complication rates have generally been reported in cases of full-arch rehabilitation, mainly consisting of fracturing/chipping of the veneering material (33.3% at 5 years), prosthetic screw fracture and screw loosening (10.4% and 9.3%, respectively, at 5 years), and hypertrophy/hyperplasia of soft tissue (13% at 5 years).4 More recently, other complications have been noted in the literature, including the opening of interproximal contacts between adjacent implants and natural teeth, and excess cement leading to peri-implantitis. This article focuses on complications commonly seen with fixed implant restorations and how to avoid such problems and treat them when they do occur.
Fracture/Chipping of the Veneering Material
With 5-year complication rates from 3.2% to 25.5%,1 chipping of the veneering material (Figure 1) is the most common technical complication addressed in the literature.1,2 This can be minimized by designing the prosthesis before the final fabrication to ensure optimal framework design and thickness of the veneering material. Following basic occlusal principles in implant prosthodontics is essential. These include reduced cuspal inclination, narrow occlusal table, correction of load direction, reduced nonaxial loading, reduced length of the cantilever, and lighter occlusal contacts on implants.5 Restorations such as monolithic zirconia (Figure 2) and lithium disilicate are also being used to minimize chipping. However, long-term follow-up information on these restorations is limited.
Screw and Abutment: Loosening and Fracture
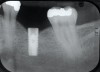
Screw loosening and fracture (Figure 3 and Figure 4) have been consistent problems in implant dentistry.6 Several adaptations have been made to the screw and implant design to minimize these issues, such as the transition from an external to internal connection and changing both the screw composition and coating. Implant manufacturers offer various implant connection and screw designs, and these designs are modified as newer and enhanced materials become available.
Even with these advances, screw loosening and fracture are common. Five-year rates of screw loosening have been 0% to 5.8%.1 Factors that can contribute to this problem include a framework that does not passively fit, biomechanical overload, improper implant positioning, repeated tightening of the screws, inadequate tightening of the screws, settling of the screws, and improper screw design.7-9
One of the best methods to avoid screw and abutment complications is to virtually plan the prosthetic design of the implant crown(s) with a prosthetically driven treatment approach using cone-beam computed technology beginning at the time of surgery. Even with virtual planning, however, the implant may be placed at an angle that is not in the axial direction of the adjacent teeth or the direction of the occlusal load. The direction of force and screw-access location must also be taken into consideration. The dentist must be diligent about verifying the integrity of the screw and abutment and ensuring that the prosthetic components are appropriate for the implant being restored, ie, a final screw is used rather than a laboratory screw (Figure 5 and Figure 6).
The use of third-party vendors for prosthetic components should be avoided.10 Third-party components (Figure 7) typically do not fit to the same standards as the manufacturer’s recommendations and can, thus, both weaken the screw connection before the screw is even placed in function and introduce micromotion that may lead to fracture of the implant or the screw/prosthesis, or crestal bone loss.11,12
The implant crown should also be verified with a stock analogue to determine the proper seating and confirm that the abutment has not been damaged. A new screw should also be provided. When the crown is being adjusted for fit intraorally, the number of times the implant screw is torqued must be kept to a minimum. Torqueing the screw more than 10 times can cause permanent elastic deformation, thus increasing the risk for screw loosening and fracture.13
If an implant crown does come loose, the cause must be determined. A radiograph should be exposed to establish that the problem resides with the prosthetic components rather than with an implant failure. Various techniques have been described in the literature for removing cement-retained restorations. If the crowns have been cemented with permanent cement or are otherwise not retrievable, one can check if the original implant cast is available. If so, a guide can be made by creating a stent over a duplicate of the final restoration and retrofitting the stent over the original cast to identify the screw-access hole location.14,15 If the original cast is unobtainable, an access hole can be made by judging the implant angulation on a radiograph.9 As a last resort, the implant crown may have to be sectioned. Several techniques have also been developed to aid in crown retrieval such as lingual retaining screws,16 applying stains to the screw-access location,17 or using an angulated screw-channel restoration.
Once the screw has been located, it should be examined for damage under a microscope. In cases with multiple units using prosthetic screws such as fixed dentures (hybrids), the screws are subject to galling (adhesive wear). Screws located anterior to the fulcrum line will wear and deform at a faster rate than those posterior.18 As the screw preload (clamping force) is lessened, more adhesive wear of the screw is observed. It should be noted that the screw preload has been shown to decrease over time.12 Clinicians may want to consider retightening or replacing screws at the subsequent recall appointment following insertion of the definitive prosthesis.19
Fractured screws are challenging to retrieve, particularly when they are abutment screws. If the screw head is accessible, a hemostat can be used to remove it. However, when the screw breaks inside the implant (Figure 8 and Figure 9), removal can be highly complicated in order not to damage the implant’s internal threads. Therefore, many implant manufacturers have developed screw-retrieval kits. Because it is critical to be able to visualize the area, magnification using loupes and a surgical microscope may be necessary.8 Additional methods can be used to remove the fractured screw. A ¼ round bur set on a high speed can be used by lightly activating it, touching only the side of the screw. After repeating this technique several times, the screw may be able to be backed out with an explorer tip. Ultrasonic tips with copious irrigation may also dislodge the screw.7,20 In cases in which this fails, a small slot can be made in the head of the screw to back it out.21 If screw threads have been damaged during retrieval, they may be retapped using a tool obtained only from the implant manufacturer.7
The increase in demand for esthetically pleasing implant restorations has led clinicians to embrace the use of all-ceramic abutments. This has subsequently increased abutment fractures (Figure 10 and Figure 11)22,23 and decementation of the ceramic crown and corresponding abutment.24 Use of zirconia abutments is relatively new in implant dentistry and has limited long-term follow-up data. Time will tell whether this technology is successful.
Excess Cement Leading to Peri-implantitis
If all implant-supported crowns could be designed for screw retention, no discussion of excess cement would be necessary. However, screw retention is not always possible depending on the location of the access opening and because of the unesthetic appearance in anterior restorations or the mesial/distal angulation of the implant compromising the path of insertion (Figure 12). Residual cement left after crown cementation on implants can lead to peri-implant inflammation, peri-implantitis, and eventual loss of the implant (Figure 13 through Figure 15).25 The presence of lingering excess cement can encourage the development of bacterial colonization and peri-implantitis. Conversely, when too little cement is used, voids in the cement layer can occur and the prosthesis can become loose.26 The deeper the implant crown margin, the more difficult it is to remove excess cement.27
Radiopaque cements that contain zinc phosphate and zinc oxide (with and without eugenol) should be considered to help identify excess interproximal cement; however, this should be used secondarily to proper margin height and careful removal of cement during cementation. Resin cements lack the same opacity as zinc-containing cements and have been shown to be the most difficult to remove.28 Often in the process of removing this excess cement, the abutment surface becomes scratched and damaged, potentiating further plaque accumulation.29
Several modifications in abutment design and cementation have been suggested. Placing vent holes in the abutment during fabrication or leaving most of the screw-access chamber open for access has reduced the amount of cement that expresses out into the sulcus.26 It is also beneficial to extraorally express excess cement on an abutment replica prior to final crown seating to minimize complications. If retrievability is desired with cementable implant crowns, weaker cements (eg, zinc oxide eugenol) should be used first and progressively changed until the desired retention is achieved.
Open Proximal Contacts
During the initial planning phase for implant therapy, the dental practitioner should not assume that the existing position of the teeth within the dental alveolus will remain stationary throughout the patient’s lifetime. Long-term follow-up of implant restorations has proven that often it does not remain stationary, regardless of the age of the patient. Open contacts have frequently been reported between implants and adjacent teeth.30
Open proximal contacts between implants and adjacent teeth have been attributed to ongoing craniofacial growth31 and vector forces mesializing tooth position (Figure 16 and Figure 17).32 These changes, particularly in the esthetic zone, can contribute to differences in incisal edge position, gingival margin height, and the facial contour and alignment of the dental arch (Figure 18 and Figure 19).31 Jemt et al30 studied a population of 28 consecutive anterior implant crowns followed for 15 years. During this time, only 8 patients demonstrated no movement of the adjacent teeth; 55% of adjacent teeth displayed palatal tooth movement, predominately in the female population.30 Shifting of teeth can contribute to occlusal changes leading to uneven occlusal load and distribution among the arch.31 Similar to adjacent open contacts between teeth, any open contact can lead to food impaction/accumulation, pocketing, and inflammation of the interdental tissue.
Greenstein et al32 made several suggestions for the treatment of open interproximal contacts, including discussing with the patient prior to treatment the possibility that therapy may be needed for the implant crown. Also, the need for retrievability of the crown should be considered so that porcelain may be added to the crown, and adjacent teeth should be modified to include broad, flat contacts. In addition, in circumstances when the crown cannot be removed, the contacts may be added to the adjacent teeth.
Conclusion
According to the complications consensus of 2014,33 prosthetic complications can be minimized by planning appropriate implants and prosthetic designs for each case, following the manufacturers’ instructions for all prosthetic components, carefully assessing and checking for misfit of the framework, and monitoring occlusal forces. In addition, greater caution should be taken with ceramic abutments because long-term data on their use do not exist, and clinicians should be aware of their specific material requirements. Also, providing an adequate framework to reduce the likelihood of veneering materials chipping. Furthermore, the full contour of the finished prosthesis should be determined before completing the underlying framework to ensure adequate thickness of the veneering material. Patients should be monitored at regular recall appointments, which should be increased in number depending on case complexity, and these appointments should include a careful occlusal analysis.
In addition to these considerations, the clinician must take into account future retrievability as it has become increasingly apparent that the craniofacial region is far from static. Screw-retained restorations or careful cementation with temporary cement should be considered. In cases in which permanent cementation is indicated, a radiopaque cement should be used and the master cast should be maintained if future access to the screws is ever indicated.
Disclosure
The authors had no disclosures to report.
About the Authors
Elyce E. Link-Bindo, DMD
Private Practice in Prosthodontics
Doylestown, Pennsylvania
James Soltys, DDS
Associate Professor
Eastman Institute for Oral Health
University of Rochester
Rochester, New York
Private Practice in Prosthodontics
Victor, New York
David Donatelli, DDS
Assistant Professor
Temple University Kornberg School of Dentistry
Philadelphia, Pennsylvania
Richard Cavanaugh, DDS
Adjunct Clinical Professor
Temple University Kornberg School of Dentistry
Philadelphia, Pennsylvania
Private Practice in Prosthodontics
Doylestown, Pennsylvania
Queries to the authors regarding this course may be submitted to authorqueries@aegiscomm.com.
References
1. Pjetursson BE, Asgeirsson AG, Zwahlen M, Sailer I. Improvements in implant dentistry over the last decade: comparison of survival and complication rates in older and newer publications. Int J Oral Maxillofac Implants. 2014;29 suppl:308-324.
2. Goodacre CJ, Kan JY, Rungcharassaeng K. Clinical complications of osseointegrated implants. J Prosthet Dent. 1999;81(5):537-552.
3. Wittneben JG, Buser D, Salvi GE, et al. Complication and failure rates with implant-supported fixed dental prostheses and single crowns: a 10-year retrospective study. Clin Implant Dent Relat Res. 2014;16(3):356-364.
4. Papaspyridakos P, Chen CJ, Chuang SK, et al. A systematic review of biologic and technical complications with fixed implant rehabilitations for edentulous patients. Int J Oral Maxillofac Implants. 2012;27(1):102-110.
5. Koyano K, Esaki D. Occlusion on oral implants: current clinical guidelines. J Oral Rehabil. 2015;42(2):153-161.
6. Zarb GA, Schmitt A. The longitudinal clinical effectiveness osseointegrated dental implants: the Toronto study. Part III: problems and complications encountered. J Prosthet Dent. 1990;64(2):185-194.
7. Imam AY, Moshaverinia A, Chee WW, McGlumphy EA. A technique for retrieving fractured implant screws. J Prosthet Dent. 2014;111(1):81-83.
8. Patel RD, Kan JY, Jonsson LB, Rungcharassaeng K. The use of a dental surgical microscope to aid in retrieval of a fractured implant screw: a clinical report. J Prosthodont. 2010;19(8):630-633.
9. Patil PG. A technique for repairing a loosening abutment screw for a cement-retained implant prosthesis. J Prosthodont. 2011;20(8):652-655.
10. Jabbari YS, Fournelle R, Ziebert G, et al. Mechanical behavior and failure analysis of prosthetic retaining screws after long-term use in vivo. Part 4: failure analysis of 10 fractured retaining screws retrieved from three patients. J Prosthodont. 2008;17(3):201-210.
11. Jabbari YS, Fournelle R, Ziebert G, et al. Mechanical behavior and failure analysis of prosthetic retaining screws after long-term use in vivo. Part 2: metallurgical and microhardness analysis. J Prosthodont. 2008;17(3):181-191.
12. Jabbari YS, Fournelle R, Ziebert G, et al. Mechanical behavior and failure analysis of prosthetic retaining screws after long-term use in vivo. Part 3: preload and tensile fracture load testing. J Prosthodont. 2008;17(3):192-200.
13. Guzaitis KL, Knoernschild KL, Viana MA. Effect of repeated screw joint closing and opening cycles on implant prosthetic screw reverse torque and implant and screw thread morphology. J Prosthet Dent. 2011;106(3):159-169.
14. Doerr J. Simplified technique for retrieving cemented implant restorations. J Prosthet Dent. 2002;88(3):352-353.
15. Kheur M, Harianawala H, Kantharia N, et al. Access to abutment screw in cement retained restorations: a clinical tip. J Clin Diagn Res. 2015;9(2):17-18.
16. Chee WW, Torbati A, Albouy JP. Retrievable cemented implant restorations. J Prosthodont. 1998;7(2):120-125.
17. Schwedhelm ER, Raigrodski AJ. A technique for locating implant abutment screws of posterior cement-retained metal-ceramic restorations with ceramic occlusal surfaces. J Prosthet Dent. 2006;95(2):165-167.
18. Jabbari YS, Fournelle R, Ziebert G, et. al. Mechanical behavior and failure analysis of prosthetic retaining screws after long-term use in vivo. Part 1: Characterization of adhesive wear and structure of retaining screws. J Prosthodont. 2008;17(3):168-180.
19. Katsuta Y, Watanabe F. Abutment screw loosening of endosseous dental implant body/abutment joint by cyclic torsional loading test at the initial stage. Dent Mater J. 2015;34(6):896-902.
20. Walia MS, Arora S, Luthra R, Walia PK. Removal of a fractured dental implant screw using a new technique: a case report. J Oral Implantol. 2012;38(6):747-750.
21. Williamson RT, Robinson FG. Retrieval technique for fractured implant screws. J Prosthet Dent. 2001;86(5):549-550.
22. Aboushelib MN, Salameh Z. Zirconia implant abutment fracture: clinical case reports and precautions for use. Int J Prosthdont. 2009;22(6):616-619.
23. Ferrari M, Tricarico MG, Cagidiaco MC, et al. 3-year randomized controlled prospective clinical trial on different CAD-CAM implant abutments. Clin Implant Dent Relat Res. 2016 Mar 14. doi: 10.1111/cid.12418.
24. Schepke U, Meijer HJ, Vermeulen KM, et al. Clinical bond Ving of resin nano ceramic restorations to zirconia abutments: a case series within a randomized clinical trial. Clin Implant Dent Relat Res. 2015 Oct 12. doi: 10.1111/cid.12382.
25. Linkevicius T, Puisys A, Vindassiute E, et al. Does residual cement around implant-supported restorations cause peri-implant disease? A retrospective study. Clin Oral Implants Res. 2013;24(11):1179-1184.
26. Wadhwani C, Hess T, Piñeyro A, et al. Cement application techniques in luting implant-supported crowns: a quantitative and qualitative survey. Int J Oral Maxillofac Implants. 2012;27(4):859-864.
27. Linkevicius T, Vindasiute E, Puisys A, et al. The influence of the cementation margin position on the amount of undetected cement. A prospective clinical study. Clin Oral Implants Res. 2013;24(1):71-76.
28. Wadhwani C, Hess T, Faber T, et al. A descriptive study of the radiographic density of implant restorative cements. J Prosthet Dent. 2010;103(5):295-302.
29. Agar JR, Cameron SM, Hughbanks JC, Parker MH. Cement removal from restorations luted to titanium abutments with simulated subgingival margins. J Prosthet Dent. 1997;78(1):43-47.
30. Jemt T, Ahlberg G, Henriksson, Bondevik O. Tooth movements adjacent to single-implant restorations after more than 15 years of follow-up. Int J Prosthodont. 2007;20(6):626-632.
31. Daftary F, Mahallati R, Bahat O, Sullivan RM. Lifelong craniofacial growth and the implications for osseointegrated implants. Int J Oral Maxillofac Implants. 2013;28(1):163-169.
32. Greenstein G, Carpentieri J, Cavaliaro J. Open contacts adjacent to dental implant restorations: Etiology, incidence, consequences, and correction. J Am Dent Assoc. 2016;147(1):28-34.
33. Heitz-Mayfield LJ, Needleman I, Salvi GE, Pjetursson BE. Consensus statements and clinical recommendations for prevention and management of biologic and technical implant complications. Int J Oral Maxillofac Implants. 2014;29 suppl:346-350.