You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
In any clinical situation, complete mouth rehabilitation starts with a comprehensive analysis of the total oral environment.1 This is developed by examining how to establish an optimum plane of occlusion, occlusal vertical dimension (OVD), occlusal scheme, and esthetics for a proper prosthetic rehabilitation.1 To do this, the clinician must depend on an adequate collection of prosthodontic data that includes: 1) personal, medical, dental, and prosthetic histories; 2) necessary radiographs; 3) articulated dental casts; and 4) a visual and digital extraoral and intraoral clinical examamination.2
Clinicians often underestimate the practical usefulness of articulated dental casts. Doing so can result in unforeseen future treatment problems and poor outcomes. These preliminary study casts are articulated at the correct therapeutic OVD in a retruded contact position (RCP), on a semi-adjustable articulator using an adjusted ear-facebow, and often a protrusive record.1 Occlusal surfaces’ harmony between any type of prostheses and the remaining natural teeth is an important factor in the preservation of the surrounding oral tissues.
One of the final goals in complete mouth treatment is to establish a satisfactory articulation. This is done by: 1) evaluating the existing occlusal scheme; 2) correcting the existing occlusal disharmony; 3) recording a retruded physiologic jaw position; 4) recording eccentric jaw relations; and 5) correcting occlusal discrepancies created by the fit of the final prosthesis. Many occlusal schemes are described in the dental literature and practiced every day. There is no scientific evidence that supports one occlusal scheme over the other.3 Where anterior guidance must be reestablished or where it changes, there currently appear to be more authorities who favor canine guidance over group function.3 For complete dentures, most prosthodontists use a balanced type of occlusal scheme. It is very apparent that the location of the centric relation (CR) or retruded contact jaw position is an important step for the application of any occlusal scheme.
The purpose of this article is to present a predictable and easy manner in which to locate and register a centric or retruded and eccentric physiologic jaw position when fabricating removable prostheses.
Review of Literature
The literature on centric relation is vast, and the definition and methods of attaining and recording CR have long been controversial. In the Glossary of Prosthodontic terms, published periodically by the Academy of Prosthodontics, the definition of CR has changed often. The 2005 edition of that publication4 has seven definitions for centric relation. It is defined as “the maxilla-mandibular relationship in which the condyles articulate with the thinnest avascular portion of their respective discs with the complex in the anterior-superior position against the shapes of the articular eminencies. This position is independent of tooth contact. This position is clinically discernible when the mandible is directed superior and anteriorly. It is restricted to a purely rotary movement about the transverse horizontal axis.”4 Additionally, Jasinevicius et al5 found in their study on the definitions of centric relation taught in seven US dental schools that there was no consensus definition.
The centric relation concept has had many revisions, perhaps more than any other in the field of dentistry. The CR record is considered by many to be the most important and most difficult maxillo-mandibular relation record to make.6 For this reason, many methods in the dental literature for recording CR records have been suggested. The categories of CR recording are as follows7:
Direct interocclusal records. Known as the “mush-squash” bite, the direct interocclusal recording was described by P. Pfaff in the 1700s. It was obtained by placing soft warm wax or modeling compound between the edentulous ridges and asking the patient to bite and “squash” the wax to a “comfortable” jaw position. Hanau and Wright improved the technique in the 19th century.
Functional recordings. Functional recordings or “chew-in” records were first described in 1910. Needles used studs mounted on record bases to engrave arrow tracings into compound rims in the mandibular arch. Boos developed the gnatho-dynamometer to determine where the maximum biting force could be. He claimed that the optimum occlusal position and the position of the maximum biting force are coincident.
Cephalometrics. Cephalometric recordings of CR and OVD were originally determined by using radiographs. The technique was described by Pyott and Schaeffer in 1952. Due to the patient’s excessive exposure to radiation, the practice of this technique was not popular.
Intraoral and extraoral graphic recordings. Graphic recording methods result in a Gothic arch tracing of mandibular movements. The intersection of the arcs produced by the right and left working movement form the apex that indicates the most retruded jaw position. The recordings can be made intraorally (Figure 1) or extraorally depending on where the records are placed.
The earliest graphic tracings were made by Balkwill in 1866 to study mandibular movements, then improved by Hess, Gysi, and Sears around 1925. In 1929, Hall modified the method to use a central bearing screw to help equalize the pressure on the supporting structure. Phillips developed a tripoded ball bearing mounted on a jackscrew for the mandibular occlusion rim. It was called “central bearing point.”
The techniques for CR recording used in dentistry today have evolved and are the results of many improvements and modifications of old CR records techniques. Schweitzer stated that most experienced dentists may not be able to give a precise definition of this controversial position, but for the average patient, they should be able to record it.8 This is because of many various factors that influence the recording of CR, including: pain in the temporomandibular joint (TMJ) or masticatory system, protective reflexes caused by faulty occlusal contacts, emotional stress, recording media, guidance or manipulation by the clinician, and neuromuscular conditioning.7
In teaching prosthodontics and when describing any technique of CR recording, it is difficult to convince clinicians or dental students that the technique will cause the condyles to articulate with the thinnest avascular portion of their respective discs with the complex in the anterior-superior position against the slopes of the articular eminencies. In addition, it has been argued that anterior disc position is a variant of normal disc position and it has been challenged: “…not all discs displaced are associated with derangement or other joints pathosis”9 and “…50% of the condyles do not seat.”10
The authors propose, from a clinical standpoint, the use of the term retruded contact position (RCP) instead of an anatomical definition of CR or centric occlusion (CO). RCP is defined clinically as retruded, unstrained, repeatable position and where the mandibular movements start. With this definition, it is easy to select a clinical technique that meets all the requirements of such position. As is known, repeatability remains the most suitable and accepted method for evaluating a mandibular record to be used for the articulation of a dental cast, denture fabrication, and occlusal equilibration. If a mandibular record is not reproducible, then the dentist cannot evaluate treatment outcomes. Celenza said: “the precision of the position may be more important than the position itself.”11
Central Bearing Device
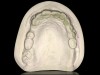
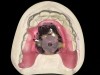
For the above reasons the authors have selected the use of Gothic arch tracings made by a central bearing device for the determination of such a mandibular jaw position. The central bearing device has a long history in dentistry. Because of the many various such devices that have been available over the years some confusion and misuse has resulted. However, with recent developments and refinements, the authors suggest that dentistry revisit this issue in light of the concept that more than one use is applicable. Use of a central bearing device during maxillo-mandibular record-making for edentulous patients has been discussed in great detail over the years. A study by Keshvad and Winstanley12 showed that of three CR methods evaluated, the bimanual manipulation method positioned the condyles in the TMJ with a more consistent repeatability than the other two methods, whereas Gothic arch was the least consistent method. However, because the complete denture record bases are movable, the present authors have found that utilizing the jaw recorder provides ease of obtaining a physiological RCP or CR. When used during complete denture therapy, it is generally believed that the central bearing device provides equalization of occlusal pressure and increases record base stability when denture-bearing mucosal resiliency is modest (Figure 2). Additionally, when the bearing plate is inked prior to placement, unguided mandibular movements through all eccentric positions will result in a Gothic arch tracing by the central bearing point on the bearing or striking plate. The apex of this tracing may then be used to identify the RCP, right and left excursions, and protrusive along the borders of the tracing (Figure 3). A thin plastic pin receiver plate single perforation or a divot prepared with a round bur into the bearing plate can be used to let the patient hold this position at the apex while registration material is being placed (Figure 4). This Gothic arch tracing method and maxillo-mandibular registration technique is considered highly reliable, even for inexperienced operators, if used at a given vertical dimension.13 In dentate or partially edentulous patients or patients with implants supporting a removable prosthesis, this method increases the reliability of the record by not allowing any tooth contact, which may deflect mandibular movements.
There are numerous advantages of such a record, including its repeatability. Also, with the use of a flat platform, the reflex pattern of closure or engram will be forgotten. Additionally, the apex of the tracings is easy to identify and represents the retruded contact jaw position, and attaining a protrusive record is easily and accurately done when indicated. Finally, it can be used in many different clinical situations and at different stages in prosthesis fabrication. Examples of these situations include during recording the RCP and also during placement of the prosthesis to correct some occlusal discrepancies or to do a clinical remount.
The jaw relation recording device (Figure 5) used by the authors is composed of five parts14:
Parallel spacer plate. This plate assists the practitioner in placing the maxillary striking plate and mandibular pin receiver parallel to each other and provides enough pin room to take the recording.
Small and large striking plate. These are smooth-surfaced plates attached to the maxillary record base with light-cured material, sticky wax, compound, or adhesives.
Small and large pin receiver. These are attached to the mandibular record base with light-cured material, sticky wax, compound, or adhesives. The nut and pin are snapped into the center socket of the pin receiver.
Nut. The pivoting nut is inserted into the pin receiver socket.
Pin. The pin is screwed into the nut. This assembly permits rotation that helps adjust the pin perpendicular to the striking plate after the bases are placed into the mouth. This is a unique feature of the jaw relation recording device.
Clinical Applications of Jaw Relation Recording Device
Clinical Application 1
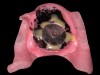
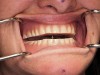
Recording RCP for fabrication of immediate dentures is depicted in Figure 6 through Figure 16. Maxillary and mandibular definitive master impressions are made with vinyl polysiloxane (VPS) material in special thermoplastic stock trays (eg, Strong-Massad Impression Tray, Nobilium, www.nobilium.com). Master impressions are poured in type III stone (eg, Microstone, Whipmix, www.whipmix.com) to generate master casts. Denture record bases (eg, Triad®, DENTSPLY Prosthetics, www.dentsply.com) are fabricated for the maxillary and mandibular casts to take the jaw relation records. The record bases must be stable and appropriately extended, and must not impinge on any frenum or vestibular attachments. The jaw relation recording device assembly is attached to the maxillary and mandibular record base with light-cured material, autopolymerizing acrylic as per manufacturer’s recommendations. The maxillary and mandibular record bases with the attached intraoral tracer assembly are placed in the patient’s mouth. In order to determine the patient’s correct RCP, the mandible must be vertically positioned at the desired OVD. To determine the OVD accurately, the rest vertical dimension (RVD) must first be determined.
The RVD is determined by marking a dot on the tip of the patient’s nose and another dot on his or her chin (Figure 10). The patient is then asked to take a deep breath and relax, and when the patient is fully relaxed, the caliper is used to record the distance between the two dots. This measurement represents the patient’s tentative physiological rest position.14,15 The pin height on the jaw relation recording device is adjusted to touch the maxillary striking plate at this measurement. This technique is useful in helping to determine a clinically acceptable OVD.
The next step is to adjust the pin height of the jaw relation recording device to OVD. A generally appropriate OVD is 2 mm to 4 mm less than the RVD. After recording the RVD and adjusting the pin to the striking plate at RVD, the pin on the jaw relation recording device is lowered by 2 mm to 4 mm, stabilizing the patient’s jaws at this critical vertical position. The patient is instructed to close slowly until the tip of the threaded pin touches the striking plate. The OVD is assessed at this point and if it is found to be optimal, the striking plate is covered with an indelible ink. The patient is trained and directed to make all border movements while maintaining contact between the vertical pin and the striking plate. These movements produce an arrow-shaped tracing. The apex of the arrow indicates the RCP position. An interocclusal record is taken at the established OVD with the patient in RCP position with a VPS bite registration paste (such as Regisil®, DENTSPLY Caulk, www.caulk.com). Registration is facilitated by affixing a centrally perforated, thin clear plastic disc over the apex of the tracing. This helps the patient hold the position at the apex, while registration material is polymerizing.
Clinical Application 2
The next application for the jaw relation recording device is for establishing OVD and recording RCP in patients needing full-mouth rehabilitation and immediate dentures. The procedure is the same as described in Clinical Application 1. Most of these patients are overclosed due to excessive tooth wear and need an increase in OVD for optimal restoration of function and esthetics. RCP records have to be made at the restored OVD. This can be most accurately achieved using the jaw relation recording device. Also, this method increases the reliability of the record by not allowing any tooth contact, which may deflect mandibular movements.
Clinical Application 3
Balance of complete dentures, removable partial dentures, and implant overdentures (Figure 17) is another application. One of the most difficult procedures in removable prosthodontics is finely equilibrating the occlusion of the finished prosthesis. Intraorally, the prosthesis moves with every occlusal prematurity, producing erroneous marks on the articulating paper. Extraoral remounts are time-consuming and often incorporate inaccuracies, due to the remount procedure itself. The jaw relation recording device eliminates these problems.16
When mounted on the finished prostheses, the pin and striking plate of the jaw relation recording device perform two functions. They act as a central bearing point, stabilizing the prostheses through constant, centralized pressure. Secondly, the pin can be adjusted until the teeth are slightly apart, and then slowly closed (with the mandible in RCP position.) Through this gradual closure, the smallest occlusal prematurity can be seen, marked, and appropriately adjusted. This process is continued until occlusion is adequate and equal on both sides of the arch.
Clinical Application 4
Yet another application involves fabrication of an occlusal splint to reposition the mandible in a physiologic position.14 Many patients present with a severely overclosed jaw position with their existing dentures (due to prolonged wear of the same set of dentures). In these patients, habitual positioning of the mandible and neuromuscular programming make it difficult to accurately record RCP position.14 It is important to return the facial musculature to the proper vertical position prior to final RCP recording. Massad et al have described the fabrication of an occlusal splint (utilizing the patient’s existing dentures), which helps reposition the mandible at the optimal OVD.13 It is fabricated by the functionally generated path method14,17,18 using the jaw relation recording device. The device is mounted on the patient’s current prostheses as per manufacturer’s recommendation (Figure 18 and Figure 19). The pin/striking plate relationship is adjusted until the patient’s jaws are held at the desired OVD. The mandible is positioned in RCP and the space between the maxillary teeth and the mandibular posterior teeth is analyzed. If this space is less than 2 mm to 3 mm, the mandibular prosthetic teeth are adjusted accordingly with laboratory rotary instruments.
The maxillary posterior teeth are lubricated with a lubricant (eg, Reline Screen, LeeMark Dental, www.leemarkdental.com). Autopolymerizing tooth-colored acrylic resin (eg, Jet Acrylic, Lang Dental Manufacturing Co., www.langdental.com) is mixed, and the “doughy” resin is placed over the mandibular posterior teeth. While the acrylic is in a doughy consistency, the patient is instructed to perform all the mandibular movements (keeping contact of the pin with the striking plate at the predetermined OVD). This movement is continued until the initial set of the acrylic. The splint is removed from the mouth and then placed in a pressure pot (eg, Polyclav®, Dentaurum, www.dentaurum.de) containing warm water for 20 minutes and is pressurized at 25 psi. Next, laboratory rotary instruments are used to trim excess acrylic. The patient is instructed to wear the splint until stable maxilla-mandibular relationship can be recorded. The splint will help deprogram the muscle and also enable the patient to get accustomed to the new OVD.
Conclusion
The jaw relation recording device presented in this article is an intraoral graphic recording device that results in a tracing of mandibular movements in one plane with the apex of the tracing indicating the RCP position. The device can be used in many different clinical situations and at different stages in prosthesis fabrication, including: recording RCP; adjustment of occlusion at time of delivery of the prosthesis; as a substitute for a clinical remount procedure; and occlusal equilibration.
Disclosure
Dr. Massad is the designer and patent holder of the jaw recorder discussed in this article. The other authors had no disclosures to report.
About the Authors
Tony Daher, DDS, MSEd
Associate Professor
Department of Restorative Dentistry
Loma Linda University
School of Dentistry
Loma Linda, California
William A. Lobel, DMD
Clinical Associate Professor
Department of Diagnosis and Health Promotion
Tufts University School of Dental Medicine
Boston Massachusetts
Joseph Massad, DDS
Clinical Associate Professor
Department of Prosthodontics
University of Tennessee Health Science Center
Memphis, Tennessee
Adjunct Associate Professor
Tufts University School of Dental Medicine
Boston, Massachusetts
djunct Associate Professor
Department of Comprehensive Dentistry
University of Texas Health Science Center Dental School
San Antonio, Texas
Adjunct Associate Professor
Department of Restorative Dentistry
Loma Linda University, School of Dentistry
Loma Linda, California
Swati Ahuja, BDS, MDS
Adjunct Assistant Professor
Department of Prosthodontics
University of Tennessee Health Science Center
Memphis, Tennessee
Zarko Jack Danilov, CDT
Owner
Danilov Dental Laboratory
Carmichael, California
Queries to the author regarding this course may be submitted to authorqueries@aegiscomm.com.
References
1. Daher T, Hall D, Goodacre CJ. Designing successful removable partial dentures. Compend Contin Educ Dent. 2006;27(3):186-193.
2. McGivney GP, Carr AB. McCracken’s Removable Partial Prosthodontics. 7th ed. St. Louis, MO: Mosby; 1985:195.
3. Thornton LJ. Anterior guidance: group function/canine guidance. A literature review. J Prosthet Dent. 1990;64(4):479-482.
4. The glossary of prosthodontic terms. J Prosthet Dent. 2005;94(1):10-92.
5. Jasinevicius TR, Yellowitz JA, Vaughan GG, et al. Centric relation definitions taught in 7 dental schools: results of faculty and student surveys. J Prosthodont. 2000;9(2):87-94.
6. Holden JE. Centric relation treatment position concepts and related research. Lecture handout presented at: ACP Center for Prosthodontic Education; 2007.
7. Myers ML. Central relation records-historical review. J Prosthet Dent. 1982;47(2):141-145.
8. Schweitzer JM. Dental occlusion: a pragmatic approach. Dent Clin North Am. 1969;13(3):687-724.
9. Stegenga B, de Bont LG, Boering G. van Willigen JD. Tissue responses to degenerative changes in the temporomandibular joint: a review. J Oral Maxillofac Surg. 1991;49(10):1079-1088.
10. Scapino RP, Mills DK. Disc displacement internal derangements. In: McNeill C, ed. Science and Practice of Occlusion. Chicago, IL: Quintessence Books; 1997.
11. Celenza FV. The centric position: replacement and character. J Prosthet Dent. 1973;30(4 Pt 2):591-598.
12. Keshvad A. Winstanley RB. Comparison of the replicability of routinely used centric relation registration techniques. J Prosthodont. 2003;12(2):90-101.
13. el-Aramany MA, George WA, Scott RH. Evaluation of the needle point tracing as a method for determining centric relation. J Prosthet Dent. 1965;15(6):1043-1054.
14. Massad JJ, Connelly ME, Rudd KD, Cagna DR. Occlusal device for diagnostic evaluation of maxillomandibular relationships in edentulous patients: A clinical technique. J Prosthet Dent. 2004;91(6):586-590.
15. Niswonger ME. The rest position of the mandible and the centric relation. J Am Dent Assoc. 1934;21(9):1572-1582.
16. Wojdyla SM, Wiederhold DM. Using intraoral Gothic arch tracing to balance full dentures and determine centric relation and occlusal vertical dimension. Dent Today. 2005;24(12):74-77.
17. Meyer FS. A new, simple and accurate technique for obtaining balanced and functional occlusion. J Am Dent Assoc. 1934;21:195-203.
18. Meyer FS. Balanced and functional occlusion in relation to denture work. J Am Dent Assoc. 1935;22(7):1156-1164.