You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
Three major elements are in the macro-esthetic paradigm: the skeletal component, dento-alveolar aspect, and facial soft-tissue envelope. Dentists are expected to use these parameters to reestablish proper masticatory function and achieve patient satisfaction. Although facial esthetic preferences can be influenced by many other external factors, it is assumed that if the jaws are proportionally related to the face and each other in all three dimensions and if the dentition is positioned correctly in these jaws, then the soft tissue should drape esthetically.1,2 The remaining esthetic problems will be influenced by the micro-esthetic issues: incisor display, dental midlines, incisor inclination, posterior functional occlusal plane, and gingival levels, as well as shade, contour, and arrangement.3 If the facial architectural framework can be changed to its physiologically correct position, dentists can not only improve patients’ appearances but also improve health. It is becoming clear that physical, emotional, and psychological health is intimately related to cranio-mandibular architecture.
Case Report
While on a medical mission to Dominica in the West Indies, a 22-year-old male presented to the outpatient clinic in November 2006 with the chief complaint that his lower jaw had been slowly changing for the past 3 to 5 years. These changes had produced severe facial distortions and interfered with his mastication (Figure 1). The findings of a clinical examination revealed a large, painless, and expansive lesion in the left mandible. The round, tan and black/brown tumor was focally fungating and extending from the left first molar to the first premolar on the opposite side. The tumor infiltrated and distorted a portion of the mandibular bone and extended to the medial floor of the mouth. Numerous teeth had been displaced anterolaterally; the most noticeable were the incisors, canines, and first premolars (Figure 2).
Because the problem was extensive and complex, the patient was transferred to a large academic medical center for definitive treatment and rehabilitation.
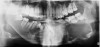
At that appointment, a cone-beam computed tomography (CBCT) scan and other radiographs were obtained. The radiographic findings revealed a multilocular expansile radiolucency that extended further than what was observed in the initial clinical examination. The radiolucency appeared to displace the inferior alveolar canal and lower border and had expanded but not perforated the mandibular cortex (Figure 3). The diagnostic work-up initially consisted of lesion aspiration. Then, multiple pieces were collected by incisional biopsy. The pathology report showed the histologic presence of epithelial islands that mimicked the enamel organ within a fibrous collagenized stroma. There were peripheral columnar cells resembling preameloblasts, a loose arrangement of epithelial cells with squamous metaplasia, and cystic degeneration toward the center (Figure 4). These histopathologic findings were consistent with the diagnosis of primary invasive ameloblastoma.4
Typically, an ameloblastoma is a benign, infiltrating neoplasm of the mandible or maxilla that, if neglected, can cause severe facial disfigurement and functional impairment. Slow growth and painless swelling are characteristic. The mass is locally invasive and progressive but also can be destructive. This epithelial odontogenic tumor of the jaws has a high rate of recurrence if not removed adequately but has virtually no tendency to metastasize. Curative treatment of a primary invasive ameloblastoma is accomplished by performing a segmental mandibulectomy for tumor ablation using a bony safety margin of 1.0 cm to 1.5 cm. Enucleation and curettage are not advised because recurrences and tumor seeding develop.4,5
Mandibular reconstruction occurred in June 2007. All remaining lower teeth were removed, and a subtotal mandibular resection was performed to remove the ameloblastoma, which extended from slightly below the left mandibular condyle to the right angle of the mandible (Figure 5). The tumor was removed intact; it measured 10.2 cm x 7.4 cm x 7.1 cm. Mandibular reconstruction can be challenging for the surgeon wishing to restore its unique geometry; however, reconstruction can be achieved with titanium bone plates followed by autogenous bone grafting. In this case, incorporation of the bone graft into the mandible provided continuity and strength required for primary esthetics and function and permitted dental implant rehabilitation at a later stage.
Rapid prototyping technology was used to construct physical models from a computer-aided design.6 A prefabricated 3D model was constructed, which assisted in the accurate contouring of titanium reconstruction plates (TRPs) and allowed planning of the actual bone graft harvest geometry before surgery. These 3D models were fabricated before the resection of the mandibular ameloblastoma; they were used to simulate the surgery and prepare the TRPs before the first stage of reconstruction.
The titanium bone plates were placed to stabilize the segments. This was followed by the placement of freeze-dried cadaver bone that served as a crib to receive milled autogenous bone chips. Perforations were made on the freeze-dried cadaver bone crib, which was then contoured to fit the defect and held in place by the custom-made titanium plates fixed with screws on both ends (Figure 6). Particulate bone chips from the anterior and posterior iliac crests were mixed with autogenous platelet-rich plasma (PRP). The mixture of bone and PRP was packed into the defect under the titanium plates to fill dead spaces and interfaces. The addition of PRP appears to accelerate the repair process and enhance early autologous graft healing.7,8 Three months after reconstruction, 10 to 12 endosseous implants were to be inserted.
Prior to implant placement, the vertical dimension of occlusion had to be reestablished and a new functional posterior occlusal plane developed. Within this framework, the axial position of the implants could be established. However, the positions of these implants were not solely predetermined by the bony architecture of the newly reconstructed mandible but also could be altered to conform to the proportional harmony of the lower face. To assist in this determination, a left lateral skull film was obtained (Figure 7) and an analysis of facial form, vertical dimension, and incisor position was performed. It was determined that the vertical dimension of the lower face would need to be increased; the posterior occlusal plane would need to be intruded; and the axial position of the lower incisor implants would have to be upright over the newly augmented ridge. In order to establish an esthetic anterior occlusal plane, the upper incisors would have to be retracted without extrusion.9 Final vertical dimension was confirmed by a CBCT scan with a modified surgical guide in place (Figure 8), and this same guide was used for the placement of 10 endosseous dental implants. Then, a transitional lower denture was fabricated and orthodontic treatment was instituted while the implants were allowed to integrate.
The initial intraoral photograph of the maxillary teeth showed the severity of the dental protrusion, the incisor irregularity, and a dual plane of occlusion. It was evident that the premolars and molars were extruded relative to the incisor esthetic plane (Figure 9). Orthodontic appliances were placed and the maxillary left and right first bicuspids extracted. To establish adequate posterior anchorage for the incisor retraction and the molar intrusion that would be necessary, a 1.6 mm x 8 mm temporary anchorage device (TAD) was placed bilaterally in the buccal-attached gingiva between the roots of the first and second molars.10,11 Care was taken to avoid contact with and not abrade the cementum in this interradicular area.12 Nickel titanium 12-mm closed coils were attached from each TAD to the orthodontic arch wire directly between the lateral incisors and canines (Figure 10). The unique mechanical properties of superelasticity and shape memory exhibited by nickel titanium supplied the constant physiologic force necessary for en masse anterior tooth movement.13 The maxillary incisors were placed in the desired axial and anteroposterior position that would be consistent with the axial placement of the endosseous dental implants in the anterior reconstructed mandible (Figure 11). By these movements, the esthetic occlusal plane and incisor display were established.
In August 2007, an implant-supported transitional prosthesis was fabricated and the initial functional occlusal plane established.14 There was a noticeable tilting downward of the maxillary first and second molars with an apparent lack of interocclusal space for lower implant-supported rehabilitation. Then, the second molars were included in the orthodontic appliance and a stiff-yet-resilient orthodontic arch wire was placed with an intrusive vertical force vector. In a sling-like arrangement, these elastic modules were attached to the same TADs previously used for incisor positioning (Figure 12). The posterior functional occlusal plane was altered by the intrusion of the maxillary first and second molars and stabilized by adjusting the implant-supported transitional prosthesis.15,16 At treatment completion in November 2009, the orthodontic appliances were removed and implant-supported prosthetic rehabilitation was continued (Figure 13).
Discussion
To assess the macro-esthetic changes that have occurred within the skeletal, dental, and facial structures after the removal of the large ameloblastoma, photographic and radiographic images will be examined in this discussion. The images are from two periods: the first was taken immediately after the subtotal mandibular resection and surgical reconstruction and the second after orthodontic and restorative dental rehabilitation. Each is used to illustrate the 3D esthetic changes that occurred.
After surgical resection, the transverse dimensions were proportional and the facial deformation had been greatly improved; however, the vertical dimension of the lower face had been decreased. This decrease was manifested mostly below the upper lip where the maxillary dental protrusion, increased tooth exposure at rest, a distorted lower lip, an everted lower lip trapped under the upper incisors, a deep labiomental fold, and poor chin definition could be seen (Figure 14). However, when the vertical dimension was reestablished by a transitional prosthesis on the surgically reconstructed mandible, other distortions were evident: a severe maxillary dental protrusion, a poor functional occlusal plane, lip incompetence, and the inability to achieve lip closure (Figure 15).
The maxillary dental movements and mandibular prosthetic reconstruction were necessary to achieve a further macro-esthetic refinement. These additional soft-tissue esthetic changes resulted from the placement of 10 endosseous dental implants with implant-supported prosthesis and by the vertical and anteroposterior orthodontic movement of the maxillary teeth (Figure 16). In November 2009, it was observed that the vertical proportionality of the lower face had been normalized, as well as the lip closure ability, lower lip distortion, deep labiomental fold, and chin prominence (Figure 17).
Conclusion
To execute multidisciplinary care for complex dentofacial abnormalities, a team must develop a consistent philosophy and mission regarding examination, diagnosis, and treatment-planning procedures. By beginning with esthetics and taking into consideration the impact on function, structure, and biology, the clinician will be able to use various disciplines in dentistry to deliver the highest level of care to each patient.17,18 After surgical segmental mandibulectomy for tumor ablation, patients often have disfigurements, thwarted function, and psychosocial problems. Multidisciplinary rehabilitation that establishes early functional and esthetic recovery offers many advantages. It aims to restore oral health, facial esthetics, and quality of life. The multidisciplinary approach not only provides the best outcomes for the patient but also may be the most efficacious and cost-effective way for meeting treatment goals.
References
1. Ricketts RM. Divine proportion in facial esthetics. Clin Plast Surg. 1982;9(4):401-422.
2. Maganzini AL,Tseng YK, Epstein JZ. Perception of facial esthetics by native Chinese participants by using manipulated digital imaging techniques. Angle Orthod. 2000;70(5):393-399.
3. Kokich VG. Esthetics and vertical tooth position: the orthodontic possibilities. Compend Contin Educ Dent. 1997;18(12):1225-1231.
4. Marx RE. Invasive ameloblastoma. In: Marx RE, Stern D, eds. Oral and Maxillofacial Pathology: A Rationale for Diagnosis and Treatment. Hanover Park, IL: Quintessence; 2003:645-648.
5. Pogrel MA, Montes DM. Is there a role for enucleation in the management of ameloblastoma? Int J Oral Maxillofac Surg. 2009;38(8):807-812.
6. Schuckert KH, Jopp S, Teoh SH. Mandibular defect reconstruction using three-dimensional polycaprolactone scaffold in combination with platelet-rich plasma and recombinant human bone morphogenetic protein-2: de novo synthesis of bone in a single case. Tissue Eng Part A. 2009;15(3):493-499.
7. Camarini ET, Zanoni JN, Leite PC, et al. Use of biomaterials with or without platelet-rich plasma in postextraction sites: a microscopic study in dogs. Int J Oral Maxillofac Implants. 2009;24(3):432-438.
8. Gerard D, Carlson ER, Gotcher JE, et al. Effects of platelet-rich plasma on the healing of autologous bone grafted mandibular defects in dogs. J Oral Maxillofac Surg. 2006;64(3):443-451.
9. Di Paolo RJ, Philip C, Maganzini AL, et al. The quadrilateral analysis: an individualized skeletal assessment. Am J Orthod. 1983;83(1):19-32.
10. Cope JB. Temporary anchorage devices in orthodontics: a paradigm shift. Semin Orthod. 2005;11:3-9.
11. Poggio PM, Incorvati C, Velo S, et al. “Safe zones”: a guide for miniscrew positioning in the maxillary and mandibular arch. Angle Orthod. 2006;76(2):191-197.
12. Renjen R, Maganzini AL, Rohrer MD, et al. Root and pulp response after intentional injury from mini-screw placement. Am J Orthod Dentofacial Orthop. 2009;136(5):708-714.
13. Maganzini AL, Wong A, Ahmed M. Forces of various nickel titanium closed coil springs. Angle Orthod. 2010;80(1):182-187.
14. Fueki K, Kimoto K, Ogawa T, et al. Effect of implant-supported or retained dentures on masticatory performance: a systematic review. J Prosthet Dent. 2007;98(6):470-477.
15. Vecchiatini R, Mobilio N, Barbin D, et al. Milled bar-supported implant overdenture after mandibular resection: a case report. J Oral Implantol. 2009;35(5):216-220.
16. Chiapasco M, Colletti G, Romeo E, et al. Long-term results of mandibular reconstruction with autogenous bone grafts and oral implants after tumor resection. Clin Oral Implants Res. 2008;19(10):1074-1080.
17. Winter RR. Interdisciplinary treatment planning: why is this not a standard of care? J Esthet Restor Dent. 2007;19(5):284-288.
18. Spear FM, Kokich VG. A multidisciplinary approach to esthetic dentistry. Dent Clin North Am. 2007;51(2):487-505.
About the Author
Anthony L. Maganzini, DDS, MSD, Director of Orthodontics, Montefiore Medical Center, The Center for Craniofacial Disorders, The Children’s Hospital at Montefiore, Bronx, New York; Professor, Albert Einstein College of Medicine; Private Practice, Bronx, New York