You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
Every dentist recognizes the importance of occlusion for clinical success in dentistry, yet very few take the necessary steps to understand and control its impact objectively in everyday practice. Most dentists are aware of the ongoing debate over whether it is more important to treat just the teeth, the muscles, or the joint as the Rosetta stone of occlusion. However while dentists acknowledge that they need to know more, it is hard to know where to start.
This article outlines a strategy to address occlusion using biometrics. Biometrics is the gathering of objective data from the patient’s stomatognathic system. Biometrics is used widely throughout all fields of medicine. The term refers to the gathering of recordable, measurable, and reproducible data from the patient. Blood pressure, cholesterol levels, and blood chemistry are only a few examples of recordable biometric data that physicians routinely gather to evaluate, diagnose, and treat patients. The significance of being able to record data for analysis, comparison, and archiving cannot be overstated. This is what elevates occlusal analysis to a true science as compared with subjective analytical methods.
Generating recordable data is important, and recordable, objective data points cannot be obtained with articulating paper. Historically, articulating paper has been used as the sole instrument for gathering data from the patient’s occlusion. However, it is impossible to use articulating paper to obtain specific defined data to measure, archive, compare, and study occlusion. This fact alone prevents research to obtain parameters to analyze, study, and therefore, standardize the use of articulating paper. In contrast, using biometrics in dentistry does provide objective data that has been studied, researched, and evaluated for more than 40 years. Research has defined specific pathologies related to the objective data obtained from biometrics. Therefore, a clear and objective understanding of the interrelationships that exist with the teeth, muscles, and joints of the patient is now possible with a high degree of accuracy. This data and its accuracy provide practitioners with the ability to evaluate, diagnose, and treat occlusion as never before.
Biometrics has three distinct relevancies with regard to occlusion: diagnosis, treatment, and reevaluation. With a more accurate diagnosis, the dentist can define the current state of the patient’s stomatognathic system, and therefore, treatment plan with greater clarity and purpose. The subsequent treatment is guided by the objective data and feedback from biometrics. Finally, the dentist has a very powerful tool to reassess the outcome and determine with objectivity whether the intended treatment goals were obtained. These data help the dentist clearly diagnose and understand the patient’s occlusion.
THE BIOMETRIC APPROACH
The approach described in this article is simple for patients to understand and accept, straightforward for the office to implement into its busy workflow, and easily performed by auxiliaries, increasing productivity of the practice. This model encompasses all three aspects of the stomatognathic system including the teeth, muscles, and joints, which interrelate and define a patient’s occlusion. This approach overcomes the difficulty often encountered helping patients to realize their condition and the complex nature of occlusion. Additionally, it is easily accessible, and can be applied purposefully to all dental patients. When used proactively, clinicians can catch potential problems early, often preventing many overlooked and debilitating conditions. This approach also provides for scalable treatment that is driven by patients and built on objective data and findings, not a subjective belief system, which unfortunately is necessary when diagnosing in the absence of data.
Step One
A biometrics approach begins with joint vibration analysis (JVA). The BioJVA™–Quick test (BioResearch Associates Inc, Milwaukee, WI) is a computer-assisted vibration analysis of the patterns of friction and vibration, which should be performed routinely on every dental patient. JVA has been shown to be 98% sensitive and 98% specific in the diagnosis of joint pathology.1,2 Simply stated, this means it has the ability to show both the true presence and absence of disease. Further, a JVA is easy to replicate and allows different practitioners the ability to obtain the same diagnosis 98% of the time. This is in contrast to 14% and 48% consistency of diagnosis with the respective use of a stethoscope or Doppler ultrasonography.3-5 The ability to diagnose the condition of the joint easily and accurately is significant because, as early as 1984, an American Dental Association committee stated in its findings that dentists should be the primary source of evaluation and treatment of temporomandibular disorders (TMDs).6 Since then, various researchers, committees, and organizations have echoed these sentiments to the dental profession. Yet, overwhelmingly, most practitioners continue to provide little if any assays or treatment for joint-based diseases and occlusion. In less than 2 minutes, a wealth of information can be obtained with the BioJVA–Quick test. The BioJVA–Quick test uses industry-unique and patented accelerometers that are arranged as a very simple headset.
Using a JVA recording device provides the practice with a tool for better patient understanding of occlusion through heuristics. The power of heuristics is well understood through the research of ethologists, scientists who study human behavior. According to Cohen,7 individuals in a busy society, such as United States, are so overwhelmed with stimuli and information that they often take shortcuts, even to many very personally relevant daily decisions. This could be one reason many practices find it difficult, if not impossible, to help patients understand (let alone treat) occlusal-based issues. The BioJVA–Quick test provides patients with information and objectivity that allows self-discovery and makes the connections so critical for codiagnosis. This happens because of heuristics where patients see objective and accurate data on the computer screen and easily recognize and understand their condition. It has been shown that involving patients and providing objective data, as opposed to hearing only the subjective perspective of the provider, are powerful triggers that help patients decide on the relevancy of information received and act on a particular topic.8
The specific triggers that the BioJVA–Quick test provides are consistency of application, involvement and commitment, integrity and authority, proof of value, and allowance for objection-raising within a noncommittal environment.9 More specifically, when patients recognize that the provider uses and consistently applies these technologies for every patient, it helps them understand the value it potentially holds for their care. Being able to give patients objective data that illustrates and quantifies an issue that is often overlooked consequently builds patient confidence in the dentist’s abilities to potentially treat these conditions. With this information, there is often a flood of questions previously withheld regarding these issues, allowing patients the opportunity to explore, raise questions or objections, and codiagnose these issues without bias. These psychological triggers provide patients with information they easily and comfortably accept, and then act upon.
Step Two
If the patient and practitioner further decide to explore and possibly treat a positive finding from the JVA, full biometric testing is recommended. Full biometric testing provides the dentist with accurate data regarding the interrelationships of the teeth, muscles, and joints. These data allow the dentist to understand how these elements of occlusion influence and affect each other within the individual’s stomatognathic system and treatment plan accordingly. Full biometric testing can be performed by the support staff and be reviewed later by the dentist. This allows auxiliaries to become more productive assets within the practice. Full biometric testing is also invaluable to reevaluate the patient after the proposed treatment to assess the outcome or success of therapy objectively and quantitatively. Based on the findings of the biometric testing, the clinician can determine the state of health of the patient’s stomatognathic system accurately. By diagnosing and isolating any discrepancies of the teeth, muscles, or joints, the practitioner can guide the appropriate treatment for that patient. Whether a single-unit or a full-reconstruction case, biometric testing offers dentists the ability of assaying for degenerative joint disease before treatment, which may influence the clinician’s and patient’s ultimate decisions. Additionally, with this data the dentist can become proactive with treatment planning to help stabilize the patient’s stomatognathic system, potentially preventing difficult-to-treat degenerative conditions from occurring.
FURTHER BIOMETRIC TESTING
If it is determined that full biometric testing is required, the clinician can examine objectively the timing and force of individual tooth contacts by using the T-Scan® III (Tekscan Inc, South Boston, MA), a USB computerized scanning device. The clinician also can record craniofacial muscle activity in both rest and function by using the BioEMG™ II (BioResearch Associates Inc). Then, through the use of T-Scan/BioEMG Link software (Tekscan Inc/BioResearch Associates technology partnership), the clinician can determine the specific activity of the muscles of mastication timed exactly with the individual contact forces.
THE BENEFITS OF SCIENTIFIC ACCURACY
Almost universally dentists use articulating paper and centric occlusion as their basis for performing, analyzing, and delivering dentistry. With biometric testing, dentists can obtain objective and concise results that help diagnose, treat, and reevaluate a patient’s occlusion and stomatognathic system. The use of articulating paper alone for occlusion fails to follow the basic tenets of the scientific method on which all research and modern advancements are based. The definition of the scientific method from the Encyclopedia Britannica reveals that for a hypothesis to be tested, one needs to collect objective, recordable, reproducible data. This allows for a process called “full disclosure,” which is critical so that others may replicate the same results for additional analysis at different times and locations.10 Imagine how difficult it is to describe and subsequently share in a quantitative, objective manner the markings made with articulating paper to a colleague in a different state or country. Unfortunately, there are no studies to verify or show how articulating paper alone can provide for these specific requirements of the scientific method. Kerstein et al11 have shown there is a very poor correlation of the actual marks made with articulating paper and the specific force creating them. Even more disturbing was their finding that higher forces often paradoxically leave less ink markings on the tooth surface. This author, as well as other dentists, has noted with use of the T-Scan III that often areas of greater force indicated with the device appear less densely marked with articulating paper. This is noted routinely with a wide variety of papers and articulating films. This phenomenon and direct comparison is easily noted by users of the T-Scan III device because it is necessary to use articulating paper in conjunction with the device, whose mylar sensor does not make any physical markings on the tooth surface during its use. Articulating paper is necessary after a scan to indicate the actual force and timing events noted with the T-Scan III.
Case 1: Scientific Articulation
The following case illustrates the concerns about using articulating paper alone for occlusion. The patient had an all-ceramic restoration placed to fix a previously fractured tooth. This case initially was completed before using an objective scanning device for occlusion analysis. The all-ceramic crown failed shortly after placement. Figure 1 shows the subsequent replacement crown immediately after milling and before characterization, glazing, and final insertion. Checking the occlusion with 20-μm articulating paper produced what appeared to be very light contact on tooth No. 31. Figure 2 shows the subsequent T-Scan III analysis of the same patient.
The computerized analysis showed that even with very light articulating paper markings there were excessive forces being placed on the area around tooth No. 31. The 3D graph showed the exact area that needed to be adjusted for this discrepancy. Because this area of concern was previously undetectable with articulating paper alone, it may be the cause of the initial failure of the patient’s tooth. The new all-ceramic crown placed after using T-Scan III analysis and adjusting the occlusion based on the finding solved this problem. Whereas the original restoration fractured within 1 month, the subsequent replacement, as of this writing, has lasted for more than 2 years without failure.
Often material choice alone is considered the primary factor to take into account with fracturing or occlusion-based issues. If clinicians simply attempt to repair damage with a material they believe less likely to fracture again, they can overlook the possible cause of the failure. While that approach may seem to solve the fractured tooth concern initially, occlusal forces could displace as problems to other teeth, muscles, and/or joint of patients. Biometrics allows clinicians the ability to analyze occlusion objectively and address the cause instead of just treating the effect. These tools allow dentists to practice comprehensively on the entire stomatognathic system instead of simply repairing damage.
This allows delivery of biologically based, instead of just spatial, dentistry. Occlusion is not influenced solely by the restoration material used in the previous example; therefore, the failure of the initial crown should not be attributed to the inherent qualities of all-ceramic crowns versus porcelain-fused-to-metal (PFM) crowns or gold crowns. The properties of current ceramic materials often closely match the original properties of natural enamel.12 An intrinsic characteristic and property of ceramics is that they are brittle, much like a natural tooth, whereas gold or metal is ductile and not as prone to failure by fracture. Therefore, ceramics are likely to fail by fracturing whereas an all-gold restoration, or the metal framework of a PFM, is unlikely to fail immediately. Unfortunately, merely masking the occlusal discrepancies does not remove these forces. Therefore, if a clinician overcomes the fracturing through material choice, he or she is ignoring these forces. Occlusal force discrepancies often show up as issues elsewhere in the stomatognathic system. The many benefits of using all-ceramic materials can be realized when biometrics are used to address the forces of occlusion. Simply changing materials might eliminate a chronic fracturing problem, but without an objective analysis the new restoration may create an uncomfortable tooth, muscles of mastication, etc. Grinding the tooth further out of occlusion can solve this problem only for the short term because eruption likely will cause the discrepancies to return.
Case 2: Full Occlusal Rehabilitation
The following case illustrates how the biometric approach can be used along with the tenets of both popular schools of thought regarding occlusion. In this example coordinating the timing and activity of individual muscles, as well as a canine-protected occlusion, will be used simultaneously to improve a patient’s overall occlusion.
A direct feedback loop exists with proprioception of teeth and the elevator muscles of mastication.13 The more teeth that contact, the higher the muscle contraction in that area increases. Group function, therefore, causes more muscle firing than single-tooth canine rise. Hyperactivity of these muscles can lead to a variety of clinical pathologies including headaches, muscle fatigue, joint dysfunction, bruxism, and tooth wear.14 After recording the timing and force of tooth contacts with the T-Scan III, and the muscle activity with the BioEMG II, the clinician can use the linking software (T-Scan/BioEMG Link) to observe the disocclusion of teeth from centricocclusion toward lateral excursions. Lessening the otherwise difficult-to-isolate interferences during this transition creates harmony in the occlusion.14 The software allows the clinician to confirm muscle activity, synergy, and symmetry as it changes from altering tooth contacts. Reducing the number of teeth contacting during this transition reduces unnecessary muscle contraction. Lessening the amount of muscle activity can be the difference between comfortable occlusion and a potential trigger for any of the previously mentioned muscle-based pathologies.14
Preadjustment, the patient experienced a left excursive from centric occlusion (Figure 3). After some initial adjustments, the software confirmed that the patient finally achieved canine rise after group function, and the elevator activity decreased accordingly (Figure 4). Then, the working and nonworking interferences were adjusted to make the transition from centric occlusion to canine rise as efficient as possible. The results of the final adjustments were confirmed with the software (Figure 5).
Computer analysis allowed the clinician to assess accurately and adjust concisely in less time only those interferences that disrupted the disocclusion of teeth from group function into canine rise. This was possible because the software showed the exact timing and specific tooth contacts and loads in conjunction with muscle activity. Reducing disocclusion time from group function to canine rise reduced interferences that disrupted the harmony of the teeth, muscles, and joint complex.
CONCLUSION
The role of occlusion is often overlooked, minimized, or ignored in many dental practices. Many dentists find it difficult to understand occlusal concepts, or perhaps cannot fathom where or how to begin to incorporate occlusal technologies into their busy practices. Implementing an easy-to-learn and easy-to-use biometric approach gives clinicians a powerful tool for incorporating occlusal analysis into their practices. Through heuristics, the BioJVA–Quick test enables the patients to make the necessary connections between occlusion and the benefits of potential treatment. Further, the biometric approach provides recordable and reproducible objective data, which can lead to improved clinical results and fewer failures. Requiring far less clinical chair time, the biometric approach gives dentists the critical information they need to create harmony of the teeth, muscles, and joint complex.
DISCLOSURE
The author has received honorariums for lecturing at insert conferences, including BioResearch Associates Inc’s annual conference. Additionally, BioResearch Associates Inc has paid the author to test/teach/certify dentists in proficiency (after their purchase) of Total BioPAK. All articles written by the author (including this one) have been without renumeration.
REFERENCES
1. Ishigaki S, Bessette RW, Maruyama T. Vibration analysis of the temporomandibular joints with degenerative joint disease. Cranio. 1993;11(4):276-283.
2. Ishigaki S, Bessette RW, Maruyama T. Vibration of the temporomandibular joints with normal radiographic imagings: comparison between asymptomatic volunteers and symptomatic patients. Cranio. 1993;11(2):88-94.
3. Hardison JD, Okeson JP. Comparison of three clinical techniques for evaluating joint sounds. Cranio. 1990;8(4):307-311.
4. Paesani D, Westesson PL, Hatala MP, et al. Accuracy of clinical diagnosis for TMJ internal derangement and arthrosis. Oral Surg Oral Med Oral Pathol. 1992;73(3):360-363.
5. Puri P, Kambylafkas P, Kyrkanides S, et al. Comparison of Doppler sonography to magnetic resonance imaging and clinical examination for disc displacement. Angle Orthod. 2006;76(5):824-829.
6. Griffiths R. Report of the President’s Conference on the Examination, Diagnosis, and Management of Temporomandibular Disorders. J Am Dent Assoc. 1983;106(1):75-77.
7. Cohen S. Environmental load and the allocation of attention. In: Baum A, Singer JE, Valins S, eds. Advances in Environmental Psychology. Vol. 1: The Urban Environment. New York, NY: Halstead Press; 1978.
8. Chaiken S, Trope Y, eds. Dual-Process Theories in Social Psychology. New York, NY: Guilford; 1999.
9. Cialdini R. Influence: Science and Practice. 4th ed. Boston, MA: Allyn & Bacon; 2001.
10.Baconian method. Encylopedia Britannica. 2008. Available at: http://www.britannica.com/eb/article-9011665. Accessed Jun 11, 2008.
11.Carey J, Craig M, Kerstein R, et al. Determining a relationship between applied occlusal load and articulating paper mark area. The Open Dentistry Journal. 2007;1:1-7.
12.Giordano R. Vita machinable ceramics. 2008. Available from: Vident, Brea, CA: http://www.vident.com/assets/downloads_ cloak/Vitablocs_2008_Giordano.pdf. Accessed Jul 2, 2008.
13.Huang X, Zhang G, Herring SW. Effects of oral sensory afferents on mastication in the miniature pig. J Dent Res. 1993;72(6):980-986.
14.Kerstein RB. Disocclusion time-reduction therapy with immediate complete anterior guidance development to treat chronic myofascial pain-dysfunction syndrome. Quintessence Int .1992; 23(11):735-747.
Ray M. Becker, DDS
Private Practice, Ellicott City, Maryland; International Certifying Instructor for Total BioPak and Biometric Technologies
|
| 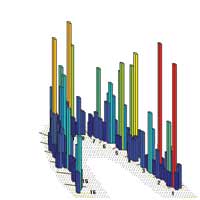 Figure 2 The T-Scan III analysis of the patient in Figure 1. Note that this method revealed excessive forces being placed on the area around tooth No. 31 (noted as ‘2’ in the figure, which represents the forces of occlusion between tooth No. 2, and the antagonist, tooth No. 31). | 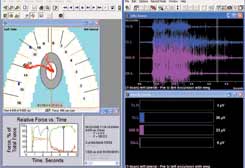 Figure 3 Preadjustment snapshot from the T-Scan/BioEMG Link software. The upper-left window showed the patient moving from centric occlusion. The lower-left window showed the excursive event took 1.296 seconds. The upper- and lower-right windows showed the prolonged muscle activity required from the elevator muscles, and significant group function with working and nonworking interferences as well as interferences and tooth contacts causing excessive muscle firing. (Case file used with permission, Robert B. Kerstein, DMD, Boston, MA.) |
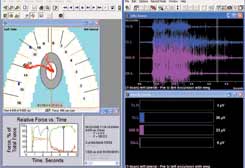 Figure 4 Preadjustment snapshot from the T-Scan/BioEMG Link software. This snapshot also shows the preadjustment state of the patient, but later in the excursive path than Figure 3. Note that there was still tooth contact on the left side in addition to the canine area (tooth No. 11) in the upper-left window. The upper- and lower-right windows showed the continued and delayed elevator muscle activity associated with this additional contact as the patient continued to move into her left lateral excursive. (Case file used with permission, Robert B. Kerstein, DMD, Boston, MA.) | 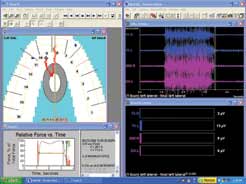 Figure 5 Postadjustment snapshot from the T-Scan/BioEMG Link software. This snapshot was produced at approximately the same timeframe after the excursive began as in Figure 3. Note the differences between views 3 and 5: The lower-left window in Figure 5 showed the time it took for the patient to perform the excursive maneuver was reduced from 1.296 seconds to 0.274 seconds. The upper- and lower-right windows showed that at the same time interval after initiating the excursive, the muscles were shutting down far more quickly and more completely than in Figure 3. (Case file used with permission, Robert B. Kerstein, DMD, Boston, MA.) |
