You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
Receiving a diagnosis of cancer can be devastating and life threatening to a patient. Dental clinicians have a duty to perform a detailed head and neck examination for any signs of malignancy. Early detection of any neoplasms enables a more favorable prognosis and conservative management. The Canadian Cancer Society estimated that in 2021, 7,400 individuals were diagnosed with head and neck cancer, 5,400 being men and 2,000 being women, with 1,500 of these individuals eventually passing away from their condition.1 In the United States, 4% of all cancers are estimated to be in the head and neck region, with more than 70,000 men and women affected by this condition in 2024.2,3 Approximately 635,000 people worldwide are affected by head and neck cancer with half of them being over the age of 60 and 21% above the age of 70.3 Currently, $8.9 billion is spent annually in the United States on the treatment and outcome of head and neck cancer.4
Head and neck cancer is defined as any neoplasms found in the oral cavity, pharynx, larynx, sinuses, and/or salivary gland. The most common type of cancer in the head and neck region is squamous cell carcinoma, with the two most prevalent sites being the oropharynx and larynx.5 Squamous cell carcinoma is more commonly found on the tongue of patients between the ages of 20 through 29, while for patients between the ages of 50 through 69 the primary location is the floor of the mouth.5 Neoplasms originating from the salivary glands account for 6% of all head and neck cancer, and cancer originating from a distant site and metastasizing to the head and neck region accounts for less than 1%.6 Most salivary gland neoplasms are found in the parotid and have a predilection of being benign, whereas tumors on the palate tend to be malignant.7 Pleomorphic adenoma is the most common salivary gland neoplasm and accounts for 70% to 94% of all salivary gland tumors.8 Moreover, hard-tissue neoplasms in the head and neck region are rare and when found are divided into odontogenic and non-odontogenic types. Studies have shown that in most patients presenting with odontogenic tumors, the tumors were benign, with the most common being an odontoma followed by an ameloblastoma.9 Osteosarcomas account for 40% to 60% of all malignant neoplasms of bone, and 10% of these cases are found in the head and neck region, primarily in the jaws.6
Pathophysiology and Histopathology
The pathophysiology of cancer involves a mutation in the cell, which causes an abnormal growth. Damage to regulatory genes can result in a cell with uncontrolled division; these genes include proto-oncogenes, tumor suppressor genes, genes that regulate apoptosis, and genes that regulate DNA repair. Furthermore, neoplasms can be classified as either benign or malignant. Benign neoplasms tend to be slow-growing, well-circumscribed, and well-differentiated and do not metastasize. Malignant neoplasms, conversely, are more aggressive having faster growth, the ability to metastasize, and cells that are poorly differentiated.
Risk factors associated with neoplasms are deemed as such because of the effect they have on genes within the cell. Tobacco and alcohol use are the major risk factors associated with head and neck cancer, with tobacco use doubling the risk for this disease.10 The use of these two substances combined leads to a synergistic effect on the risk of head and neck cancer, with one study finding a 35-fold increased risk when 84 grams of ethanol and 10 cigarettes were concomitantly consumed daily.11 After a 10-year cessation period the risk of oral cancer is reduced to that of a person who never drank alcohol or used tobacco products.12 A poor diet that lacks rich nutrients and vitamins also has been associated with an increased risk for head and neck cancer.6 Solar radiation is another risk factor for squamous cell carcinoma of the skin, with a predilection for the lower lip due to increased sun exposure.13 Genetic predisposition for head and neck cancer is also a risk factor. Patients with first-degree relatives and siblings with head and neck cancer have been shown to have a 1.7 and 2.2 increased chance of receiving a diagnosis of head and neck cancer, respectively.6 Yet another important risk factor for head and neck cancer involves microorganisms, with human papillomaviruses (HPV) 16 and 18 being highly associated with oropharyngeal and tonsillar squamous cell carcinoma.14
The gold standard method of making the diagnosis of a neoplasm is to take a biopsy; however, certain neoplasms have distinct radiographic patterns and can be diagnosed through imaging. When examining a histology specimen, benign tumors are easily differentiated from the surrounding tissue and tend to be well-demarcated with or without a fibrous capsule.15 Malignant neoplasms, to the contrary, have invasive patterns of growth, and a border surrounding the abnormal growth can be difficult to identify.15 Cells within a malignant neoplasm also have increased mitotic activity, nuclear hyperchromasia, cellular and nuclear pleomorphism, and an increased nucleus-to-cytoplasmic ratio.15
Table 1 contains various histopathologic features of common head and neck neoplasms.
Medical Management
The treatment of head and neck cancer involves removing all abnormal cells while trying to preserve as much healthy tissue as possible. Before deciding on a treatment option, the clinician must first determine the type of neoplasm present and whether it is benign or malignant and the staging. Benign tumors tend to be easier to treat and have more favorable treatment options. However, certain benign tumors, such as an ameloblastoma, require more aggressive treatment with wider margins of resection. Before choosing a treatment option for malignant neoplasms, the clinician needs to stage the cancer using the TNM criteria. The TNM criteria allows the cancer to be classified in one of the four different stages (stage 0, stage 1, stages 2 and 3, stage 4). The TNM criteria relies on three different aspects to classify the cancer: T = the size and extent of the primary tumor; N = the size, number, and location of lymph nodes; M = distant metastasis.16
Once the extent of the malignant neoplasm(s) has been identified, it can be treated via surgery, radiation, or chemotherapy. Surgery and radiation are the first treatment options for neoplasms that are in early stages. The advantage of utilizing surgery is the ability to visualize all of the malignant tumor and removing it. However, this can lead to loss of tissue and function. As the staging of the cancer is increased, more ablative and aggressive surgery will be required, which may result in additional loss of functional tissue. When nodal involvement occurs, the surgeon may need to perform neck dissections to remove all affected lymph nodes, and if the cancer is extensive radiation therapy may be required postoperatively.
When using radiation to treat cancer, conformal radiation techniques allow the clinician to target the specific areas that are malignant while preserving healthy surrounding tissue.17 For cases that are amenable to treatment with radiation only, a dosage of 50 Gray (Gy) delivered in 25 fractions over 5 weeks or 60 Gy in 30 fractions over 6 weeks may be used, and after 6 weeks if there is evidence of neoplasm remaining, surgery can be used as an adjunct.17 When postoperative radiation is used, it is usually started 3 to 4 weeks after surgery to ensure the wounds have healed, with dosages of 60 Gy over 5 weeks.17 Furthermore, brachytherapy involves placing an implantable device that emits a high dose of radiation to a small area of tissue and can be used as adjunctive treatment after surgery and radiation for any malignancy that remains after initial treatment.
Chemotherapy works by interfering with cell division at various stages. This mechanism of action is beneficial, as malignant neoplasms have uncontrolled cell division and chemotherapeutic medications can interfere with the growth of the tumor. Chemotherapeutic agents that are used in the treatment of head and neck cancer include antimetabolic agents, alkylating agents, antimicrotubule agents, antitumor antibodies, and epidermal growth factor receptor (EGFR) antibodies (Table 2).18
Antimetabolic agents are drugs that mimic molecules that are necessary for cell function; however, once incorporated into the cell, they halt cell activity. The two most common antimetabolic drugs used in head and neck cancer treatment are methotrexate and 5-fluorouracil.18 Alkylating agents work by binding and damaging DNA, which subsequently prevents enzymes necessary for cell replication to copy the genetic information. Cisplatin and carboplatin are the two most common alkylating agents used in the treatment of head and neck cancer.18 During prophase of mitosis, microtubules are formed, which are essential for the formation of mitotic spindles to allow for cell division. Vinka alkaloids and taxanes are the two antimicrotubule agents used for malignancies in the head and neck region.18 Antitumor antibodies function by inhibiting enzymes necessary for DNA replication. The enzyme that is targeted by these agents is topoisomerase, which is involved in unwinding of DNA. Lastly, EGFR is upregulated in tumors, which allows for more of the substrate (epidermal growth factor) to bind causing a secondary messenger cascade resulting in cell division. By inhibiting these receptors, the growth of the malignancy is decreased. For the management of head and neck cancer, the antitumor and EGFR antibodies used, respectively, are doxorubicin and cetuximab.
Orofacial Findings
Drastic changes in the oral cavity may occur following resective and reconstructive surgeries for head and neck cancer treatment, potentially leading to oropharyngeal dysfunction. Because of the aggressive nature of resective surgeries and loss of tissue, patients may experience problems with transient phases of swallowing, oral hygiene, self cleansability of the oral cavity, and occlusion.19 Furthermore, if the tongue is involved in the surgery, patients might experience difficulty when swallowing and/or speaking; however, if reconstructed, function can return after about a year post-surgery.20 Due to the difficulty in swallowing post-surgery, patients may experience problems eating, resulting in dependency on a gastrostomy tube.21 Moreover, the incorporation of radiotherapy postoperatively may result in subcutaneous fibrosis, trismus, and salivary gland dysfunction.22
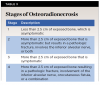
Damage to structures within the oral cavity and surrounding structures is fairly common following radiation therapy. Ulcerations may occur on the skin and mucosa. Additionally, the salivary gland is extremely radiosensitive and cell death is inevitable if it is irradiated. The patient will likely experience xerostomia resulting in difficulty eating and wearing dentures. Saliva will become thick and ropy and lose its ability to buffer acids produced by cariogenic bacteria. Therefore, patients may experience rampant decay following radiation therapy.23 The mucosa within the oral cavity can become red, inflamed, and painful, which is a condition known as mucositis, and this can result in ulceration, which subsequently can become infected. The most common location for mucositis-induced ulceration is the soft palate, although other locations are vulnerable to it as well.24 Xerostomia can exacerbate the pain caused by the mucositis. Along with the damage to the mucosa and salivary glands, blood vessels and muscles can be affected. Due to the death of muscle cells, patients may experience trismus post-radiation. Damage to blood vessels can result in loss of vitality of bone resulting in a condition known as osteoradionecrosis, defined as exposed bone through the skin or mucosa for a minimum of 3 months.25 Osteoradionecrosis is classified in stages, and as it increases in stage there is an increase in the amount of exposed bone, devitalized bone, and pathologic fractures (Table 3).26
Patients taking chemotherapeutic drugs are at risk for a decrease in production of healthy cells. If the cells originating from the bone marrow are suppressed, patients may present with a decreased amount of white blood cells, platelets, and red blood cells. When the patient becomes immunosuppressed, opportunistic infection may manifest. The most common opportunist infection seen in the oral cavity is candidiasis. Pseudomembranous candidiasis is the most common form of the infection; it presents with multiple areas of thick white film that can be rubbed off and underlying erythematous tissue. Also, viruses and bacteria can cause infection in the oral cavity in individuals who are immunosuppressed. Opportunistic infections in the oral cavity caused by virus involve herpes simplex, whereas the bacteria are Pseudomonas, Klebsiella, Proteus, Escherichia coli, and Enterobacter species.27 These infections can present as an ulcer, and the bacterial infection may not heal after the use of a broad-spectrum antibiotic treatment.27 Moreover, due to the effects chemotherapeutic agents have on dividing cells, patients on chemotherapy may also experience mucositis.
Pain is a common finding among patients with all forms of treatment for head and neck cancer as well as during the pretreatment phase. The pain experienced by the patient can be exacerbated if a multimodal treatment approach is used and can be very difficult to control, even with analgesics.28 The complex nature of the pain that can be experienced by patients has a detrimental impact on their social and physical abilities, ability to eat and take medications, and communication, all of which can compound and worsen the pain.28-30
Dental Management
Dental management of patients undergoing head and neck cancer treatment must consider the three phases of cancer treatment: precancer, intra-cancer, and post-cancer. During each phase of cancer treatment, the dental practitioner should take a thorough medical history with adequate information obtained from the oncologist. These patients may also benefit from being referred to a dental oncologist for dental treatment within a hospital setting.
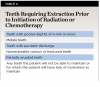
Prior to any cancer treatment, the dental clinician should thoroughly evaluate all head and neck structures. A detailed intraoral examination should be taken with appropriate radiographs, including bitewing, periapical, and panoramic images. Teeth that are nonrestorable, periodontally compromised, or have active inflammatory conditions should be extracted before the start of radiation therapy or chemotherapy. The goal for prophylactic extraction is to prevent the development of osteoradionecrosis in patients undergoing radiotherapy. However, prophylactic extractions should only be executed in areas of the jaws that will be irradiated. The threshold for prophylactic extraction is 60 Gy in the maxilla and 50 Gy in the mandible.31 Patients who are undergoing chemotherapy may develop issues with hemostasis and wound healing, which can complicate extractions. If a patient is expected to become severely immunocompromised (ie, white blood count below 2,000/µL or granulocyte count below 1,000/µL) within the following 10 days, extraction should be delayed or antibiotic prophylaxis with cephalosporins should be given.27 Teeth should be extracted at least 10 days prior to radiation and 5 and 7 days in the maxilla and mandible, respectively, prior to chemotherapy (Table 4).27 Table 5 provides a summary of threshold lab values where extractions can be safely performed and what measures should be taken if the values are below the minimum threshold. Furthermore, Figure 1 shows an algorithm with regard to proceeding with extractions in patients undergoing therapy for head and neck cancer.
During radiation therapy, the patient must follow a meticulous oral hygiene regimen. Custom fluoride trays should be fabricated for the patient prior to radiation, as damage to salivary glands can occur during radiation treatment, predisposing the patient to caries. Fluoride trays should be used for 5 minutes on clean teeth, and the patient should not eat for 30 to 60 minutes after application. Furthermore, patients should be instructed to limit cariogenic foods and use chlorhexidine 0.12% mouthrinse to limit the amount of bacteria within the oral cavity. The purpose for meticulous oral hygiene is to prevent any caries during radiation or chemotherapy. During radiation, the patient is at risk for osteoradionecrosis if any extractions are performed, with a systematic review reporting a risk of 5.8%.32 Endodontic treatment is the preferred therapy if a tooth becomes necrotic during radiation therapy. If the tooth is nonrestorable, endodontic treatment should still be carried out followed by a coronectomy. However, if the tooth absolutely needs to be extracted, a 1-week course of pentoxifylline can be used prior to extraction followed by pre- and postoperative hyperbaric oxygen.33,34 Clinicians should be cautious with this protocol as there is weak evidence to support this preventive measure and the best preventive method is to avoid dentoalveolar surgery. Furthermore, if the patient becomes immunocompromised, preventive antimicrobials can be given to reduce the risk of infection. If an infection does develop, it should be treated immediately with appropriate medication. A summary of recommended pharmacotherapy for prevention and treatment of infections following head and neck chemotherapy and radiation is presented in Table 6.27,35
Following radiation therapy, all patients should continue with meticulous oral hygiene to prevent the need for extractions. Patients should continue the use of fluoride trays with a 1.1% fluoride gel and 5,000 ppm fluoridated toothpaste. Any post-radiation caries should be restored with materials that will provide long-lasting restorations. Xerostomia should be managed with frequent sips of water and the use of xylitol gum, oral lubricants, and systemic medications (ie, pilocarpine 5 mg t.i.d., anethole 25 mg t.i.d., bethanecol 25 mg t.i.d., cevemiline 30 mg t.i.d.). Patients experiencing mucositis can manage the pain using cryotherapy and topical anesthetic solutions such as benzydamine rinses; if such conservative treatment options are ineffective, patients can be given systemic analgesics.27 Additionally, patients who have finished chemotherapy should have their blood counts measured, and if they are within normal values, no modification to dental treatment is required. If the clinician suspects that the patient has developed osteoradionecrosis, a referral should be sent to a specialist immediately. Treatments for osteoradionecrosis include pharmacological agents (eg, tocopherol, pentoxifylline, and clodronate), ultrasound therapy, hyperbaric oxygen, debridement, and resection of necrotic bone.36
Conclusion
Patients undergoing head and neck cancer treatment are at risk for various dental complications. These patient need to maintain frequent dental visits to ensure a healthy oral cavity. The dental clinician should have constant communication with the oncologist and know the patient's exact regimens and treatments. Through appropriate treatment planning, good communication, and regular dental care, the adverse effects on the oral cavity following the treatment of head and neck cancer can be mitigated.
About the Authors
Syed Salim Abdul-Wasay, DDS
Oral and Maxillofacial Surgical Resident, University of Maryland School of Dentistry, Baltimore, Maryland
Aviv Ouanounou, BSc, MSc, DDS
Associate Professor, Department of Clinical Sciences, Pharmacology and Preventive Dentistry, Faculty of Dentistry, University of Toronto, Toronto, Ontario, Canada; Fellow, International College of Dentists; Fellow, American College of Dentists; Fellow, International Congress of Oral Implantologists
Queries to the author regarding this course may be submitted to authorqueries@conexiant.com.
References
1. Canadian Cancer Statistics Advisory Committee in collaboration with the Canadian Cancer Society, Statistics Canada, and the Public Health Agency of Canada. Canadian Cancer Statistics 2021. Toronto, ON: Canadian Cancer Society; 2021. cancer.ca/Canadian-Cancer-Statistics-2021-EN. Accessed November 21, 2024.
2. Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2021. CA Cancer J Clin. 2021;71(1):7-33.
3. American Cancer Society. Cancer Facts & Figures 2024. Atlanta, GA: American Cancer Society; 2024.
4. Wissinger E, Griebsch I, Lungershausen J, et al. The economic burden of head and neck cancer: a systematic literature review. Pharmacoeconomics. 2014;32(9):865-882.
5. DiGiulio S. Oropharyngeal cancer now most common head & neck cancer. Oncology Times. 2014;36(22):96-97.
6. Bernier J. Head and Neck Cancer Multimodality Management. 1st ed. New York, NY: Springer; 2011.
7. Pouloudi D, Sotiriadis A, Theodorakidou M, et al. The impact of angiogenesis in the most common salivary gland malignant tumors. Int J Mol Sci. 2020;21(24):9335.
8. Luers JC, Guntinas-Lichius O, Klussmann J, et al. The incidence of Warthin tumours and pleomorphic adenomas in the parotid gland over a 25-year period. Clin Otolaryngol. 2016;41(6):793-797.
9. Labib A, Adlard RE. Odontogenic tumors of the jaws. 2023 Jul 10. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024. https://www.ncbi.nlm.nih.gov/books/NBK572116/. Accessed December 10, 2024.
10. Yu VX, Long S, Tassler A. Smoking and head and neck cancer. JAMA Otolaryngol Head Neck Surg. 2023;149(5):470.
11. Dal Maso L, Torelli N, Biancotto E, et al. Combined effect of tobacco smoking and alcohol drinking in the risk of head and neck cancers: a re-analysis of case-control studies using bi-dimensional spline models. Eur J Epidemiol. 2016;31(4):385-393.
12. Warnakulasuriya S, Greenspan JS. Textbook of Oral Cancer: Prevention, Diagnosis and Management. 1st ed. Cham, Switzerland: Springer; 2020.
13. Supreet BD, Mathivanan S, Merchant MI, Patil NS. Squamous cell carcinoma of lower lip reconstructed with bilateral fan flap. Ann Maxillofac Surg. 2019;9(1):211-213.
14. Andrews E, Seaman WT, Webster-Cyriaque J. Oropharyngeal carcinoma in non-smokers and non-drinkers: a role for HPV. Oral Oncol. 2009;45(6):486-491.
15. Patel A. Benign vs malignant tumors. JAMA Oncol. 2020;6(9):1488.
16. Feig BW, Ching CD. The MD Anderson Surgical Oncology Handbook. 5th ed. Wolters Kluwer/Lippincott Williams & Wilkins; 2012.
17. Alfouzan AF. Radiation therapy in head and neck cancer. Saudi Med J. 2021;42(3):247-254.
18. Ward EC, van As-Brooks CJ. Head and Neck Cancer: Treatment, Rehabilitation, and Outcomes. 2nd ed. Plural Publishing Inc; 2014.
19. Matsuda Y, Okui T, Karino M, et al. Postoperative oral dysfunction following oral cancer resection and reconstruction: a preliminary cross-sectional study. Oral Oncol. 2021;121:105468.
20. Lam L, Samman N. Speech and swallowing following tongue cancer surgery and free flap reconstruction-a systematic review. Oral Oncol. 2013;49(6):507-524.
21. Dziegielewski PT, Ho ML, Rieger J, et al. Total glossectomy with laryngeal preservation and free flap reconstruction: objective functional outcomes and systematic review of the literature. Laryngoscope. 2013;123(1):140-145.
22. Kao SS, Peters MD, Krishnan SG, Ooi EH. Swallowing outcomes following primary surgical resection and primary free flap reconstruction for oral and oropharyngeal squamous cell carcinomas: a systematic review. Laryngoscope. 2016;126(7):1572-1580.
23. Sroussi HY, Epstein JB, Bensadoun RJ, et al. Common oral complications of head and neck cancer radiation therapy: mucositis, infections, saliva change, fibrosis, sensory dysfunctions, dental caries, periodontal disease, and osteoradionecrosis. Cancer Med. 2017;6(12):2918-2931.
24. Gussgard AM, Jokstad A, Wood R, et al. Symptoms reported by head and neck cancer patients during radiotherapy and association with mucosal ulceration site and size: an observational study. PloS One. 2015;10(6):e0129001.
25. Holley T, Keenan DA, Militsakh O. Osteoradionecrosis. Current Otorhinolaryngology Reports. 2018;6(3):285-291.
26. Lyons A, Osher J, Warner E, et al. Osteoradionecrosis-a review of current concepts in defining the extent of the disease and a new classification proposal. Br J Oral Maxillofac Surg. 2014;52(5):392-395.
27. Little JW, Miller CS, Rhodus NL. Little and Falace's Dental Management of the Medically Compromised Patient. 9th ed. St. Louis, MO: Elsevier; 2018.
28. Epstein JB, Hong C, Logan RM, et al. A systematic review of orofacial pain in patients receiving cancer therapy. Support Care Cancer. 2010;18(8):1023-1031.
29. Benoliel R, Epstein J, Eliav E, et al. Orofacial pain in cancer: part I - mechanisms. J Dent Res. 2007;86(6):491-505.
30. Epstein JB, Elad S, Eliav E, et al. Orofacial pain in cancer: part II - clinical perspectives and management. J Dent Res. 2007;86(6):506-518.
31. Watson E, Mojdami ZD, Oladega A, et al, Canadian Dental Oncology Network Consensus Group . Clinical practice guidelines for dental management prior to radiation for head and neck cancer. Oral Oncol. 2021;123:105604.
32. Worthington HV, Khangura S, Seal K, et al. Direct composite resin fillings versus amalgam fillings for permanent posterior teeth. Cochrane Database Syst Rev. 2021;8(8):CD005620.
33. Lyons A, Ghazali N. Osteoradionecrosis of the jaws: current understanding of its pathophysiology and treatment. Br J Oral Maxillofac Surg. 2008;46(8):653-660.
34. Nabil S, Samman N. Incidence and prevention of osteoradionecrosis after dental extraction in irradiated patients: a systematic review. Int J Oral Maxillofac Surg.2011;40(3):229-243.
35. Carvalho CG, Medeiros-Filho JB, Ferreira MC. Guide for health professionals addressing oral care for individuals in oncological treatment based on scientific evidence. Support Care Cancer. 2018;26(8):2651-2661.
36. Meleca JB, Zhang E, Fritz MA, Ciolek PJ. Overview and emerging trends in the treatment of osteoradionecrosis. Curr Treat Options Oncol. 2021;22(12):115.