You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
Disclosure: Dr. Howes is the innovator of the concept discussed but has no commercial advantage in the company or product.
The human alveolus is an intricate, nonuniform structure that encases the complex anatomy of the human dentition and critical anatomic landmarks. Teeth, particularly those in the anterior, display a slight disparity between root and crown angulations (Figure 1), imposing obstacles in implant dentistry. The replacement of lost teeth has long been a challenge. The contemporary treatment of choice in many cases is the implant-supported prosthesis (ISP), which has been in use since the discovery of osseointegration by Professor Per-Ingvar Brånemark in the 1960s.1 An osseointegrated implant provides a direct and relatively rigid connection of the implant to the bone.2 Careful surgery is required to place a titanium fixture in the correct 3-dimensional position in bone to support an esthetic and functional tooth replacement.
Achieving consistent, long-term, fully functional, maintainable, and esthetic ISPs, however, raises surgical and restorative challenges, given the anatomic constraints and harsh intraoral environment most often responsible for tooth loss. Biologic and technical complications may arise over time, including bone and soft-tissue loss, as well as prosthesis and component or fixture fracture.
Screw retention of ISPs allows for ease of retrieval during prosthetic and surgical maintenance. Enabling screw retention requires meticulous surgical planning to position the fixture providing the prosthetic needs so that the screw emerges through the cingulum of anterior teeth and the central fossae of posterior teeth.
To overcome the anatomic constraints of the tooth and alveolus, particularly after post-extraction resorption,3,4 the surgeon often must incline the implant to be safely encased within the bone. Doing so often imposes an unfavorable restorative platform angulation for a screw-retained prosthetic rehabilitation. Placing the implant to provide a more favorable angulation brings the implant into close proximity to, or can even cause perforation of, the labial cortical plate necessitating additional surgical augmentation procedures. Such procedures can be associated with higher rates of morbidity, increased costs, and longer treatment time.5 To overcome these tooth and bony anatomic constraints and meet the surgical and restorative needs of ISPs, a dual-axial implant fixture can be used.
Anatomic Constraints of the Jaws
The anatomy of the human skeleton has evolved over millennia to meet its functional needs. The craniofacial skeleton (including the maxilla and mandible) is, therefore, anisotropic and seldom, if ever, symmetrical. The alveolus forms to surround the tooth during crown and root development. The eventual complex tooth root shape and crown position are dictated by the multidirectional forces acting on the tooth, generated by the neuromuscular engrams of the tongue, lips, and masticatory and perioral musculature. The craniofacial skeleton also envelops critical anatomic structures, including nerves, blood vessels, and the sinus and nasal cavities. The ultimate anatomy of the fully developed alveolus is the result of these influences as well as the patient’s growth pattern and is, therefore, extremely complex and variable.6-8
Kan et al9 showed that in 76% to 86.5% of cases, the tooth position in the anterior maxilla is most often positioned very close to the buccal plate (Figure 1). This plate and the roots are proclined forward from the nasal spine. Consequently, together with the crown–root angulation offset, a straight implant fixture is unlikely to be able to fully satisfy both root and crown positions, particularly if the prosthesis is to be screw retained.
The posterior maxilla houses the maxillary sinus, which varies extensively between individuals in volume and anatomy. Of the two jaws, it has the poorer bone quality and quantity.10,11 The presence of the maxillary sinus can compromise bone volume.
The anterior mandible varies considerably in bone volume but is reported to have good quality and high torque values with fixture placement.12 Although it has been regarded as one of the safest areas for implant surgery, case reports have been published in which life-threatening hematoma developed in the floor of the mouth, requiring emergency tracheostomy to establish a surgical airway.13 Other studies have described neuropathic pain after surgery in the anterior mandible.14
The posterior mandible carries the inferior alveolar nerve, which can be damaged easily. Reports have shown alarming levels of trigeminal nerve injury,15 64% of which involve the inferior alveolar nerve.16 Such injuries have resulted in litigation with respect to implant surgery and management.17
Screw and Cement Retention for Implant-supported Prostheses
Some of the first ISPs, placed from 1978 to 1982, were reported to have had success rates of up to 98.9% over more than 20 years.18 The prostheses and abutments were produced for the specific purpose of full-arch rehabilitation, particularly for the difficult edentulous mandible and, later, the maxilla.
Demand soon increased for the expansion of the Brånemark osseointegration concepts into partial-arch rehabilitation and single-tooth replacement. Fixtures were then used to carry the prostheses, but the available abutment armamentarium was not suitable for such restorations and had significant esthetic limitations.19,20
The “UCLA,” or “custom,” abutment was developed to overcome the single-tooth restorative constraints of limited interocclusal and interproximal distance, implant angulation, and soft-tissue response.20 Esthetic abutments were subsequently developed to allow for more apical positioning of the porcelain margin and to maintain screw retention. Low-profile multi-unit abutments soon followed.21
Unfortunately, conventional restorative principles were applied to implant-supported single and partial restorations at first, resulting in the cementation of prostheses onto custom abutments. “C&B&I” (crown-and-bridge and implants) was a concept for incorporating dental implants into regular crown-and-bridge dentistry; it was targeted to general practitioners as well as specialists and dental laboratories.22 One of the most common reasons for choosing cement retention is the malposition of implant fixtures due to the natural and resorptive limitations of bone, which precludes appropriate angulation for regular screw retention. With uniaxial implants, the angular correction of these fixture positions takes place coronal to the bony crest (supracrestally) by way of angulated abutments (Figure 2).
Bone augmentation procedures have been described to overcome bony constraints, but there is much debate over the optimal augmentation materials and the need for multiple procedures that, as noted previously, can result in increased costs and treatment time.5,23
The literature is divided between the benefits and hazards of cement and screw retention for ISPs. A systematic review and meta-analysis by Lemos et al24 concluded that cement-retained fixed ISPs result in less marginal bone loss over follow-up periods of between 12 and 180 months, fewer prosthetic complications, and higher implant survival rates than screw-retained prostheses. In direct contrast, a systematic review with multivariate analysis by Millen et al25 concluded that for all fixed prostheses, significantly fewer biologic and technical complications were seen with screw retention. In addition, full-arch prostheses had significantly higher complication rates than single crowns.
Ma et al26 pointed out that inconsistencies in the reporting of complications associated with screw versus cement retention make comparison difficult. Though both retention systems work and no evidence is definitive, there are many reports of complications with excess cement,27 and complications with screw retention are more easily resolved due to ease of retrievability. Biologic and technical complications are common in ISPs and widely reported.28-32 Although evidence shows that complication rates have been dropping over two decades, total cumulative biologic, esthetic, and technical complication rates still have an alarming range, from 16.1% to 60.8%, with a mean of 33.3%.33
Screw retention is, therefore, rapidly becoming a preferred mechanism for ISPs. This highlights the need for clinicians to be cognizant of prosthetic considerations during surgical planning to ensure 3D implant placement that will support an esthetic, cleansable, hygienic, and functional prosthesis.
Overcoming Anatomic Constraints
Tilting of uniaxial (straight) implants to avoid critical anatomic structures has become common practice,34 but it requires angular correction to achieve a common path of insertion for multi-unit ISPs. This is traditionally achieved with angulated abutments. Systematic reviews confirm that tilting implants with angulated abutments is a successful and predictable technique that does not induce significant crestal bone alteration in the first year of function.35
The advantages of tilting implants with the use of angulated abutments include avoidance of important anatomic structures, reduction of the need for bone-grafting procedures, and, in multiple implants, an improvement of the anterior–posterior spread to reduce cantilever length.36-38 A single ISP on a tilted implant cannot readily be screw retained without compensatory custom angulation of a separate post and cementation of a separate crown. Angulated abutments, indeed, have allowed for the differential tilting of the fixture itself; however, similar to other authors,39 the present author has found them to be cumbersome, expensive, and sometimes esthetically disappointing.
A distinction must be made between the tilting of straight implants with supracrestal angle correction by way of angulated abutments and implants with subcrestal angular correction within the neck of the fixture (Figure 2). The first angulated implant was the zygomatic implant, developed by Brånemark and placed in 1991; it was designed with angular correction within the head of the implant.36 This allowed for screw retention of prostheses supported by severely tilted implants to avoid the maxillary sinus and engage the bone of the zygoma. The use of this implant has also been described extensively for the resorbed and compromised maxilla in oncology and trauma.37,38
Development of a Root Form Dual-axis Implant
Howes et al40 described the research and development of an implant with 12-degree subcrestal angular correction, originally designed to overcome the anatomic constraints of the anterior maxilla for screw retention. In this unpublished study, the authors recognized the conflict between the surgical and restorative objectives in ISPs in the anterior maxilla. The morphology of the anterior maxilla was analyzed on lateral cephalometric radiographs of 30 class I to III maxillae. In addition, the differences between the axes of the crowns and roots of 30 anterior teeth were assessed, including canines and lateral and central incisors. The root–crown offset ranged from 8 to 12 degrees (Figure 3), and the angle between the buccal plate and ideal screw axis ranged from 25.6 to 30 degrees (Figure 4). The resultant fixture design had a 12-degree angular offset between implant body and prosthetic platform, with a 0.6-mm body thread pitch to minimize apical travel per rotation. This implant is able to accommodate these angulation constraints due to the combined taper and head angulation.
Finite element studies simulating 22-degree off-axis loading of implants positioned in the anterior maxilla showed strains developed in the dual-axis implant were well below the 483 MPa yield strength of grade 4 titanium. In contrast, the simulation showed that the uniaxial implant would suffer strains well above this threshold.40
For surgical placement the dual-axis root form fixture is connected to an angle-correcting mount having a reciprocal inclination with the angulated platform of the implant enabling the fixture to be inserted in a straight axis (Figure 5 and Figure 6). An orientation dimple shows the rotational position of the implant in the bone.
This dual-axis system allows for desirable surgical placement within bone, avoiding anatomic structures such as described above and providing for the required prosthodontic needs of appropriate crown orientation and screw retention if needed. The use of this implant has been reported to yield predictable results,41-43 including a net buccal bone gain over time.44
The subcrestal angle-corrected, dual-axial implant has advanced the treatment of the anterior maxilla by reducing the need for grafting procedures and facilitating immediate loading. Good primary stability is achieved because the threads engage the palatal triangle of bone while avoiding the buccal plate. Figure 7 illustrates the advantages of a dual-axial implant over a uniaxial implant, which would require grafting to avoid apical perforation.45 The dual-axis implant allows for maintenance of the recommended 1.5 mm to 2 mm dimension between the buccal plate and the fixture.46
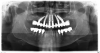
The author has used the dual-axial implant fixture unconventionally in the anterior mandible in an orientation that avoids perforation into the floor of the mouth (Figure 8).5 Dual-axial implants have also been used to avoid critical anatomic structures, such as the maxillary sinuses (Figure 9) and inferior alveolar nerves (Figure 10),47 thereby reducing the need for grafting procedures. Because these implants have subcrestal angular correction, they can be used with standard uniaxial abutments in a common path of insertion, thus enabling screw retention.
With the increased application of this concept, more options have been introduced, including 24-degree and 36-degree correction (Figure 11 through Figure 13). At present, larger angular corrections are available with external hexagon connection systems, while the 12-degree connection is also available in most internal connection configurations.
Conclusions
Surgical and prosthodontic needs in dental implantology are often in conflict due to the anatomic configurations of jaws. The dual-axis implant concept offers a resolution of these dilemmas by enabling favorable inclination of the implant in the bone, while at the same time facilitating an appropriate screw-retained prosthesis design enabled by subcrestal angular correction within the implant. In addition, more favorable biomechanics of the connections are maintained during functional loads.
Acknowledgment
Figure 2 and Figure 5 through Figure 10 courtesy of Southern Implants, South Africa. Used with permission.
About the Author
Dale G. Howes, BSc (Dent), BDS, MDent (Wits), FCD (SA) Pros, FICD Professor and Head, Department of Oral Rehabilitation, School of Oral Health Sciences, University of the Witwatersrand, Johannesburg, South Africa; Co-founder, P-I Brånemark Institute of South Africa
Queries to the author regarding this course may be submitted to authorqueries@aegiscomm.com.
References
1. Jivraj S, Chee W. Treatment planning of implants in posterior quadrants. Br Dent J. 2006;201(1)13-23.
2. Oshida Y, Tuna EB, Aktören O, Gençay K. Dental implant systems. Int J Mol Sci. 2010;11(4):1580-1678.
3. Cawood JI, Howell RA. A classification of the edentulous jaws. Int J Oral Maxillofac Surg. 1988;17(4):232-236.
4. Atwood DA. Bone loss of edentulous alveolar ridges. J Periodontol. 1979; 50(4 spec no):11-21.
5. Esposito M, Grusovin MG, Coulthard P, Worthington HV. The efficacy of various bone augmentation procedures for dental implants: a Cochrane systematic review of randomized controlled trials. Int J Oral Maxillofac Implants. 2006;21(5):696-710.
6. Moss-Salentijn L. Melvin L Moss and the functional matrix. J Dent Res. 1997;76(12):1814-1817.
7. Moss ML, Salentijn L. The capsular matrix. Am J Orthod. 1969;56(5): 474-490.
8. Moss ML, Salentijn L. The primary role of functional matrices in facial growth. Am J Orthod. 1969;55(6):566-577.
9. Kan JYK, Roe P, Rungcharassaeng K, et al. Classification of sagittal root position in relation to the anterior maxillary osseous housing for immediate implant placement: a cone beam computed tomography study. Int J Oral Maxillofac Implants. 2011;26(4):873-876.
10. Gonda T, Kamei K, Maeda Y. Determining favorable maxillary implant locations using three-dimensional simulation software and computed tomography data. Int J Prosthodont. 2017;30(1):58-61.
11. Truhlar RS, Orenstein IH, Morris HF, Ochi S. Distribution of bone quality in patients receiving endosseous dental implants. J Oral Maxillofac Surg. 1997;55(12 suppl 5):38-45.
12. Cassetta M, Sofan AA, Altieri F, Barbato E. Evaluation of alveolar cortical bone thickness and density for orthodontic mini-implant placement. J Clin Exp Dent. 2013;5(5):e245-e252.
13. Boyes-Varley JG, Lownie JF. Haematoma of the floor of the mouth following implant placement. SADJ. 2002;57(2):64-65.
14. Kütük N, Demirbaş AE, Gönen ZB, et al. Anterior mandibular zone safe for implants. J Craniofac Surg. 2013;24(4):e405-e408.
15. Juodzbalys G, Wang H-L, Sabalys G. Injury of the inferior alveolar nerve during implant placement: a literature teview. J Oral Maxillofac Res. 2011;2(1):e1.
16. Tay ABG, Zuniga JR. Clinical characteristics of trigeminal nerve injury referrals to a university centre. Int J Oral Maxillofac Surg. 2007;36(10):922-927.
17. Pinchi V, Varvara G, Pradella F, et al. Analysis of professional malpractice claims in implant dentistry in Italy from insurance company technical reports, 2006 to 2010. Int J Oral Maxillofac Implants. 2014;29(5):1177-1184.
18. Ekelund J-A, Lindquist LW, Carlsson GE, Jemt T. Implant treatment in the edentulous mandible: a prospective study on Brånemark system implants over more than 20 years. Int J Prosthodont. 2003;16(6):602-608.
19. Lewis SG, Beumer J, Perri GR, Hornburg WP. Single tooth implant supported restorations. Int J Oral Maxillofac Implants. 1988;3(1):25-30.
20. Lewis SG, Llamas D, Avera S. The UCLA abutment: a four-year review. J Prosthet Dent. 1992;67(4):509-515.
21. Kastenbaum F. Achieving ideal esthetics in osseointegrated prostheses. 1. Multiple units. Int J Periodontics Restorative Dent. 1992;12(2):153-159.
22. Nobel Biocare Holding AG Group. Nobel Biocare Full Year Report 2002. Nobel Biocare: February 2003; https://www.nobelbiocare.com/content/dam/Migration%20Assets/Documents/Discover/Company/Download%20center/Interim%20reports/2002/PR_full_year_report_2002_tcm269-28264.pdf. Accessed May 22, 2017.
23. Merli M, Merli I, Raffaelli E, et al. Bone augmentation at implant dehiscences and fenestrations. A systematic review of randomised controlled trials. Eur J Oral Implantol. 2016;9(1):11-32.
24. Lemos CA, de Souza Batista VE, Almeida DA, et al. Evaluation of cement-retained versus screw-retained implant-supported restorations for marginal bone loss: A systematic review and meta-analysis. J Prosthet Dent. 2016;115(4):419-427.
25. Millen C, Brägger U, Wittneben JG. Influence of prosthesis type and retention mechanism on complications with fixed implant-supported prostheses: a systematic review applying multivariate analyses. Int J Oral Maxillofac Implants. 2015;30(1):110-124.
26. Ma S, Fenton A. Screw- versus cement-retained implant prostheses: a systematic review of prosthodontic maintenance and complications. Int J Prosthodont. 2015;28(2):127-145.
27. Linkevicius T, Puisys A, Vindasiute E, et al. Does residual cement around implant-supported restorations cause peri-implant disease? A retrospective case analysis. Clin Oral Implants Res. 2013;24(11):1179-1184.
28. Pjetursson BE, Brägger U, Lang NP, Zwahlen M. Comparison of survival and complication rates of tooth-supported fixed dental prostheses (FDPs) and implant-supported FDPs and single crowns (SCs). Clin Oral Implants Res. 2007;18(suppl 3):97-113.
29. Pjetursson BE, Thoma D, Jung R, et al. A systematic review of the survival and complication rates of implant-supported fixed dental prostheses (FDPs) after a mean observation period of at least 5 years. Clin Oral Implants Res. 2012;23(suppl 6):22-38.
30. Goodacre CJ, Bernal G, Rungcharassaeng K, Kan JY. Clinical complications with implants and implant prostheses. J Prosthet Dent. 2003; 90(2):121-132.
31. Jung RE, Zembic A, Pjetursson BE, et al. Systematic review of the survival rate and the incidence of biological, technical, and aesthetic complications of single crowns on implants reported in longitudinal studies with a mean follow-up of 5 years. Clin Oral Implants Res. 2012;23(suppl 6):2-21.
32. Aglietta M, Siciliano VI, Zwahlen M, et al. A systematic review of the survival and complication rates of implant supported fixed dental prostheses with cantilever extensions after an observation period of at least 5 years. Clin Oral Implants Res. 2009;20(5):441-451.
33. Pjetursson BE, Asgeirsson AG, Zwahlen M, Sailer I. Improvements in implant dentistry over the last decade: comparison of survival and complication rates in older and newer publications. Int J Oral Maxillofac Implants. 2014;29(suppl):308-324.
34. Krekmanov L, Kahn M, Rangert B, Lindström H. Tilting of posterior mandibular and maxillary implants for improved prosthesis support. Int J Oral Maxillofac Implants. 2000;15(3):405-414.
35. Del Fabbro M, Bellini CM, Romeo D, Francetti L. Tilted implants for the rehabilitation of edentulous jaws: a systematic review. Clin Implant Dent Relat Res. 2012;14(4):612-621.
36. Francischone CE, Vasconcelos LW, Filho HN, et al. Prosthetic treatment of atrophic maxillae and maxillectomized patients based on osseointegration. In: The Osseointegration Book: From Calvarium to Calcaneus. Berlin, Germany: Quintessence; 2005.
37. Boyes-Varley JG, Howes DG, Davidge-Pitts KD, et al. A protocol for maxillary reconstruction following oncology resection using zygomatic implants. Int J Prosthodont. 2007;20(5):521-531.
38. Barber AJ, Butterworth CJ, Rogers SN. Systematic review of primary osseointegrated dental implants in head and neck oncology. Br J Oral Maxillofac Surg. 2011;49(1):29-36.
39. Sannino G, Barlattani A. Straight versus angulated abutments on tilted implants in immediate fixed rehabilitation of the edentulous mandible: a 3-year retrospective comparative study. Int J Prosthodont. 2016;29(3): 219-226.
40. Howes DG, Boyes-Varley JG, Blackbeard GA, Boschoff C. An angulated implant for the anterior maxilla: development and evaluation. Poster Presentation. European Association for Osseointegration Meeting, Paris, France; 2004. Proceedings published in: Clin Oral Implants Res. 2004;15:4,xi32.
41. Vandeweghe S, Cosyn J, Thevissen E, et al. A 1-year prospective study on Co-Axis implants immediately loaded with a full ceramic crown. Clin Implant Dent Relat Res. 2012;14(suppl 1):e126-e138.
42. Vandeweghe S, Hawker P, De Bruyn H. An up to 12-year retrospective follow-up on immediately loaded, surface-modified implants in the edentulous mandible. Clin Implant Dent Relat Res. 2016;18(2):323-331.
43. Boyes-Varley JG, Howes DG, Newell A, et al. A 5 to 12 year evaluation of angulated implants in various indications. Int J Oral Maxillofac Implants. Submitted for publication.
44. Brown SD, Payne AG. Immediately restored single implants in the aesthetic zone of the maxilla using a novel design: 1-year report. Clin Oral Implants Res. 2011;22(4):445-454.
45. Chan HL, Garaicoa-Pazmino C, Suarez F, et al. Incidence of implant buccal plate fenestration in the esthetic zone: a cone beam computed tomography study. Int J Oral Maxillofac Implants. 2014;29(1):171-177.
46. Chu SJ, Salama MA, Salama H, et al. The dual-zone therapeutic concept of managing immediate implant placement and provisional restoration in anterior extraction sockets. Compend Contin Educ Dent. 2012; 33(7):524-534.
47. Kurtzman GM, Dompkowski DF, Mahler BA, Howes DG. Off-axis implant placement for anatomical considerations using the Co-Axis implant. Inside Dent. 2008;12(5):96-102.