You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
Palliative care aims to provide symptom control allowing for death to occur with the least amount of distress for the patient. Palliative care dentistry has been defined as the management of patients with progressive, far-advanced disease for whom the oral cavity has been compromised either by disease or by treatment, and the focus of care is on the immediate quality of life.1 The terms palliative care and hospice care can be used interchangeably. Such care primarily involves the treatment of patients with advanced cancer, although it also extends to patients who are terminally ill with end-stage renal disease, non-cancer pulmonary disease, and terminal HIV/AIDS. This article will focus mainly on the oral care of patients with terminal cancer but will also discuss treatment options for those facing other terminal illnesses, as many such patients have oral problems that adversely impact their quality of life.
Palliative Care and Dentistry
The palliative care team traditionally includes physicians, nurses, social workers, psychologists, physical/occupational therapists, pharmacists, nutritionists, and clergy, but typically fails to include dentists. Many patients with cancer exhibit oral problems such as xerostomia, candidiasis, mucositis, and loss of masticatory function.2,3 Even with these oral morbidities, rarely is a dentist an active member of the palliative care team. Moreover, most physicians do not have the training and knowledge to provide adequate symptom relief for the array of oral maladies from which a palliative care patient suffers.
Patients with cancer of the head and neck area often experience oral problems such as xerostomia and mucositis.4,5 Any discussion of the typical oral complications associated with palliative care patients must begin with xerostomia or dry mouth. Many medications cause xerostomia, such as antidepressants, narcotics, and antiemitics. Xerostomia in patients can lead to taste alterations, candidiasis, and poor nutrition. Poor nutrition may lead to dehydration, decreased urinary output, and accumulation of opioid metabolites resulting in delirium.6 Also, poor oral hygiene often results in caries, periodontal disease, and halitosis; the latter may result in social isolation and, ultimately, depression. The oral problems suffered by palliative care patients have both a physical impact, such as difficulty with eating and drinking, opportunistic infections, mucositis, and pain, and also a social and emotional impact, including embarrassment, depression, and an inability to display emotions through actions, such as kissing.
Palliative Oral Problems
Mucositis and Stomatitis as a Result of Cancer Treatment
Therapeutic treatments for cancer include the use of or combination of chemotherapy, radiotherapy, and surgical excision. Both chemotherapy and radiotherapy may be continued during palliative care to decrease pain or improve function. Chemotherapy has a damaging effect on mitotically active sites, such as the oral cavity. The mitotic rate is higher in younger patients than in older patients.2 Radiotherapy is also damaging because it causes sclerosing of vessels, which leads to tissue atrophy.2
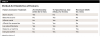
The severity of mucositis and stomatitis has been indexed by the World Health Organization. As the severity increases, the condition becomes a medical and dental emergency. Progression of the condition may lead to malnutrition and dehydration. Treatment is aimed at providing symptom relief. Pain relief can be achieved through use of various topical agents (Table 1).7-9 Many of these analgesic agents should be used with caution because they can lead to the loss of the gag reflex and can increase the potential of aspiration.10 The mouth should be kept clean and moist because mucositis and stomatitis are associated with secondary infections from microorganisms, such as fungus, bacteria, and viruses.11
Poor Nutrition
Palliative care patients are prone to anorexia-cachexia syndrome.12 Cachexia is defined as the metabolism of body tissues, especially skeletal muscle tissue, with a reduction of more than 5% of the patient’s body weight over the past 6 months. This may be associated with reduced caloric intake and systemic inflammation.13 Anorexia can be an undesirable secondary effect of many medications, including psychostimulants, antidepressants, and chemotherapy drugs. In addition, if the patient has an unhealthy oral status, eating may prove to be difficult. It has been estimated that 70% of palliative care cancer patients have anorexia.12
Xerostomia can make swallowing food difficult. Foods served moist, such as with gravy, can improve swallowing. Nutritional supplements such as Ensure® can be a good source of calories; many nutritional supplements, however, contain a high amount of fermentable sugars, putting a xerostomic patient at a greater risk for tooth decay. Non-pharmacologic approaches to improving nutrition include having patients eat small meals more frequently and making sure foods are presented to the patient in an appealing manner. Also, simply asking patients what they want to eat may help their food intake.
Dysphagia
Dysphagia affects either one or both phases of swallowing—the oropharyngeal component and/or the esophageal component. The oropharyngeal phase begins in the mouth. If the patient has an unhealthy dentition, xerostomia, or poor tongue and masticatory muscular function, then bolus formation may be difficult.14
Neuromuscular causes of dysphagia include Parkinson’s disease, cerebral vascular accident (stroke), amyotrophic lateral sclerosis, or nerve damage to the mastication muscles (ie, cranial nerves V, VII, IX, X, XI, and XII). Dysphagia may also be caused by radiotherapy to the head and neck, leading to trismus.15
Repair of carious teeth, replacement of lost teeth with partial dentures, and relining of loose dentures may improve masticatory function. In the opinion of the author, the dental care provided, besides emergency pain relief, should be based on prognostic longevity. For example, replacing missing teeth with implants and fixed prosthodontics if the prognostic period is less than a year would be unethical. An honest dialogue with the patient and his or her family is imperative before undertaking aggressive oral rehabilitation.
Esophageal phase dysfunction may be caused by physical obstruction by a tumor or by strictures induced by radiologic or surgical therapies.16,17 Consultation with a speech pathologist or an occupational therapist may assist in evaluating swallowing pathology.
Nausea and Vomiting
If helpful, chemotherapy and radiotherapy may be continued as palliative care therapies; however, nausea and vomiting are common side effects of these therapies. Other factors that occur during palliative care that increase vomiting and nausea include bowel obstruction, brain metastasis, gastroparesis, electrolyte imbalances, and opioid usage.18 The effect of chronic vomiting can be tooth erosion caused by low gastric pH, though the application of topical fluoride gels and varnishes may help protect the teeth against acid dissolution. Chronic vomiting also can result in the patient being unable to wear dentures, which may affect not only the patient’s diet (puréed versus solid food) but his or her self-image as well.
Medications used to control nausea and vomiting include scopolamine, dexamethasone, and odansetron. The former two medications have significant side effects, such as drowsiness, xerostomia, visual disturbances, and mood swings (Table 2).19-21 Natural remedies to control vomiting and nausea include ginger22 and acupuncture or acupressure,23 though the efficacy of these measures is still in question.
A major problem associated with vomiting is the loss of nutrients required for tissue repair, which could inhibit the healing of mouth sores. Furthermore, because vomiting causes dehydration and diminished urine output, opioids and metabolites may accumulate in the patient’s brain, inducing a state of delirium. Also, nausea may cause patients to forgo oral hygiene. Measures that may help reduce nausea during oral care include using a smaller, perhaps child’s size toothbrush, which may be more tolerable for the patient, and a choosing a toothpaste with a consistency and flavor that is amenable to the patient, or brushing without paste if necessary.
Xerostomia
Xerostomia, defined as the subjective sense of oral dryness, is the most common oral complaint of palliative care patients.24,25 It must be differentiated from salivary gland hypofunction, which is a quantitative measurement concerning saliva flow rate.26 Clinically, the author has encountered many patients with abundant amounts of saliva, yet they describe their mouth as dry. Conversely, a patient with a dry mouth may have no complaints. Therefore, patients may be xerostomic even if they do not have salivary gland hypofunction.
Medications are the most frequent causes of xerostomia in palliative patients.27 Other influences contributing to xerostomia include alcohol-based mouthwashes, caffeinated drinks, dehydration, and rooms with low humidity.
Saliva has many important functions, including lubrication of oral tissues, bolus formation, remineralization of teeth, and pH maintenance, as well as antimicrobial properties.28 Due to the loss of remineralization and pH buffering, patients who are xerostomic are more prone to caries, as these patients often choose foods that are soft and moist, many of which may contain high amounts of sugar and may be cariogenic.29 Palliative care patients have higher sugar taste thresholds and, therefore, may add supplemental sugar to their diets for taste.30 The use of artificial saliva agents may reduce complaints of xerostomia. The ideal saliva substitute would have a neutral pH and antimicrobial and remineralization properties, and be non-irritating, non-toxic, and pleasant tasting.
Saliva substitutes used commercially in North America are frequently carboxymethyl cellulose based and often offer relief that is short in duration. Not all commercially available artificial saliva agents have neutral pH; some have a dangerously low pH, which may increase the potential for caries.31,32 For example, pH levels of such agents can range from 3.88 (Meridol®), to 5.12 (Glandosane Spray®), to 6.89 (Oralube®).31,32
Saliva can also be stimulated using local measures, such as sugarless gums or mints, and systemic agents. Sugarless gums are favored over mints because the chewing motion promotes salivation. Flavoring agents such as cinnamon should be avoided as they may irritate fragile tissues.33 Other local measures include adhesive discs to lubricate the mouth (eg, Oramoist®, Dentek, dentek.com; XyliMelts®, OraHealth, oracoat.com)34 and water-soluble lubricants such as K-Y® Jelly (K-Y, k-y.com), Muko® Lubricating Jelly (Healthwick, healthwick.ca), Taro Gel Lubrifiant® (Taro Pharmaceutical Industries, taro.com), and Bioténe Oralbalance Moisturizing Gel® (GlaxoSmithKline, biotene.com), spread by a foam brush or finger. Systemic measures include the use of pilocarpine (eg, Salagen®) and cevimeline (eg, Evoxac®). These agents primarily act as cholinergic mimetics but have a variety of side effects such as sweating and increased pulmonary secretions. Pulmonary secretions can cause sounds during respiration, sometimes referred to as a “death rattle,” which may be distressing to palliative care patients and their families.
Finally, xerostomia can also affect denture adhesion.35 This may create a problem with mastication and can affect a patient’s self-esteem if he or she cannot wear the dentures in front of others. Having patients rinse their mouth with artificial saliva, pre-wet the denture, and use denture adhesives may aid in denture retention. Products for treating dry mouth are listed in Table 3.
Fungal Infections
Fungal infections are common in patients with xerostomia because of a microbial shift from normal to pathogenic organisms. The incidence of fungal infections in cancer patients can be as high as 57%.36 The most common fungal organism present is Candida albicans, however other organisms can be present, including Candida glabrata and Candida dubliniensis. These organisms may be resistant to fluconazole and itraconazole.37 Phenotypically, Candida infections may appear as white plaque lesions, termed pseudomembranous, or be simply erythemic, termed atrophic.38 The latter is often seen under dentures. Dentures should be treated by either soaking in sodium hypochlorite or chlorhexidine HCl 0.12%, or by a microwave. Advantages and disadvantages of each method are delineated in Table 4.39
The use of a microwave is a unique non-pharmacologic method to disinfect a denture. In one study,40 patients with type 2 diabetes and denture stomatitis were randomly distributed into two groups. The first group received nystatin topically four times a day for 14 days, and the second group had their dentures microwaved at 650W for 3 minutes three times a week for 14 days. Both groups had reduced clinical and microbiological infections. For the palliative care patient, microwaving of the dentures may be a good treatment choice when the patient becomes debilitated. Because the hyphae that have penetrated the acrylic base of the denture may still be viable, a reline may aid in decreasing reinfection.40 The addition of 800,000 IU of nystatin to the reline material can decrease reinfection.41
Treatment of fungal infections can be divided into two modalities: topical or systemic. Topical agents, which include nystatin agents and clotrimazole and miconazole products, have the advantage of acting locally with limited systemic effects. Because fungal infections can cause pain and limit nutrition, topical anesthetics may be incorporated into mixtures to decrease pain. Innovative remedies include freezing a mixture of nystatin suspension and sugar-free fruit juice into popsicles. The coldness of the popsicle may help relieve any burning sensations, and the contact time of the antifungal agent with oral tissues is increased. Moreover, the juice from the popsicle provides hydration. If the patient is semicomatose and unable to take medications by mouth because of a risk of aspiration, a 50:50 mixture of nystatin suspension with a water-soluble lubricating agent, such as K-Y Jelly, Muko Lubricating Jelly, or Taro Gel Lubrifiant, applied to the oral tissues will help treat the fungal infection.
Systemic agents include fluconazole and ketoconazole, which should be used with caution as they decrease the activity of the cytochrome P450 system (CYP3A4). Administering these antifungals can affect the metabolism of agents such as triazolam and methadone, leading to possible respiratory depression and possibly hastening death.42,43
Head and Neck Cancer
Cancer of the head and neck regions may be disturbing to the patient, the family of the patient, and the palliative care staff. With the face representing perhaps the most crucial component of body image, palliative care patients with head and neck deformities can experience both psychological and physical distress, and the care can be difficult. Head and neck cancer patients exhibit greater depression than patients with other forms of cancer.44 Depression may be treated pharmacologically with antidepressants (eg, tricyclic antidepressants, selective serotonin reuptake inhibitors, and monoamine oxidase inhibitors); a major side effect of these medications, however, is xerostomia.45 Alternatively, counseling by psychologists and hospital chaplains may decrease patient anxiety, and the use of art and music therapy may help alleviate stress in these patients. Many depressed patients might forgo their oral care, leading to increased fungal infections, mucositis, caries, and periodontal disease. Empowering family members to become active participants in the provision of oral care may lead to not only improved care but stronger patient-family bonding.
Oral Hygiene and Caries
Good oral hygiene helps prevent the secondary infections associated with mucositis and is important in preventing caries associated with a dry mouth secondary to opioid usage. Perhaps more importantly, good oral hygiene will prevent halitosis, which can affect personal relationships. Rinses that contain alcohol can further desiccate a dry mouth and should, therefore, be avoided.
If a palliative care patient develops caries, the restorative material used, in addition to being esthetic and adhesive to tooth structure, should be resistant to fracture, wear, and re-decay. Glass ionomers generally meet these criteria but may fracture in a xerostomic environment.46 Consequently, the so-called sandwich technique, in which the glass ionomer is placed first followed by a conventional composite, should be considered. If the patient, for any reason, cannot tolerate an extended period of treatment, then a temporary restorative material may be used.
Because caries may be prevented by using fluoride varnishes and gels,47,48 patients should be advised to use fluoridated toothpastes and maintain a thorough oral hygiene regimen. The author suggests that the family be involved in providing oral care to the patient to ensure it is not neglected.
Taste Alterations
Taste disorders are present in 25% to 50% of palliative care patients.49 Because the perception of taste is dependent on the dissolution of chemical mediators into saliva for the taste bud to perceive flavor, the prime cause of decreased taste is, therefore, xerostomia. Xerostomia is also a frequent side effect of head and neck radiation therapy. Radiation therapy at a dose of 20 Gy can cause taste reduction; a cumulative dose of 60 Gy will affect 90% of patients.50 Although chemotherapy creates a transient loss of taste, radiation therapy may actually cause permanent damage to the nerve–taste bud interface.51
Taste alterations may cause the patient to eat less, which may lead to dehydration. Because institutional food can often be unappealing, care should be taken to provide food for the patient in an attractive, esthetically pleasing manner, such as using tablecloths to cover food trays.
Psychological Effects
Depression may occur in patients after receiving a poor prognosis, particularly a mortality prognosis. A first-line approach in treating depression is the use of antidepressants, which may result in xerostomia.45 Depressed patients frequently neglect their oral care, and as stated earlier, poor oral hygiene leads to increased frequency of oral infections, caries, and halitosis. All of these factors may contribute to decreased social interaction by the patient, further accentuating the depression.
Depression may be reduced through good communication and listening skills by the palliative care team. Most palliative care units have chaplains available to discuss issues that may promote anxiety in palliative care patients, such as death and the afterlife. The chaplains are also important for the palliative care team to explore biomedical ethical issues, such as intravenous hydration.
Treatment Planning
Dental treatment of palliative care patients should be provided with an approach to both maintain and improve function, but with a sense of reality. The author has developed the CARE approach: The dentist must provide comfort (C) measures to maintain or improve dental function, bearing in mind that quality of life is paramount. The patient’s oral status must be continuously assessed (A) along with the changing prognosis of the patient. Finally, reality (RE) should shape the definitive treatment plan.
Conclusion
Throughout the phases of palliative care, from the time patients are active participants in their oral care to the point in which they may become comatose, the role of the palliative care dentist is to provide comfort, ensuring that the patient is free of pain and infection from dental problems, thus improving the quality of life for these patients.
About the Author
Michael Wiseman, DDS, FASGD, DABSCD, M RCS (Edin)
Associate Professor
McGill University, Faculty of Dentistry
Montreal, Quebec, Canada
Queries to the author regarding this course may be submitted to authorqueries@aegiscomm.com.
Disclosure
The author had no disclosures to report.
References
1. Wiseman MA. Palliative care dentistry. Gerodontology. 2000;17(1):49-51.
2. Sonis ST, Sonis AL, Lieberman A. Oral complications in patients receiving treatment for malignancies other than of the head and neck. J Am Dent Assoc. 1978; 97(3):486-472.
3. Sonis ST, Fey EG. Oral complications of cancer therapy. Oncology. 2002;16(5):680-686.
4. Sweeney MP, Bagg J. The mouth and palliative care. Am J Hosp Palliat Care. 2000;17(2):118-124.
5. Hanchanale S, Adkinson L, Daniels S, et al. Systematic literature review: xerostomia in advanced cancer patients. Support Care Cancer. 2015;23(3):881-888.
6. Lawlor PG. Delirium and dehydration: some fluid for thought? Support Care Cancer. 2002;10(6):445-454.
7. Epstein JB, Stevenson-Moore P. Benzydamine hydrochloride in prevention and management of pain in oral mucositis associated with radiation therapy. Oral Surg Oral Med Oral Pathol. 1986;62(2):145-148.
8. Vayne-Bossert P, Escher M, de Vautibault CG, et al. Effect of topical morphine (mouthwash) on oral pain due to chemotherapy- and/or radiotherapy-induced mucositis: a randomized double blinded study. J Palliat Med. 2010;13(2):125-128.
9. Markiewicz M, Dzierzak-Mietla M, Frankiewicz A, et al. Treating oral mucositis with a supersaturated calcium phosphate rinse: comparison with control in patients undergoing allogenic hematopoietic stem cell transplantation. Support Care Cancer. 2012;20(9):2223-2229.
10. Epstein J, Van Der Waal I. Oral cancer. In: Greenberg MS, Glick M, Ship JA, eds. Burket’s Oral Medicine. 11th ed. Hamilton, Ontario: BC Decker Inc; 2002:153-189.
11. Sonis ST. The pathobiology of mucositis. Nat Rev Cancer. 2004;4(4):277-284.
12. Yavuzsen T, Davis MP, Walsh D, et al. Systemic review of the treatment of cancer-associated anorexia and weight loss. J Clin Oncol. 2005;23(33):8500-8511.
13. MacDonald N. Terminology in cancer cachexia: importance and status. Curr Opin Clin Nutr Metab Care. 2012;15(3):220-225.
14. American Gastroenterological Association medical position statement on management of oropharyngeal dysphagia. Gastroenterology. 1999;116(2):452-454.
15. Agarwal J, Palwe V, Dutta, D, et al. Objective assessment of swallowing function after definitive concurrent (chemo)radiotherapy in patients with head and neck cancer. Dysphagia. 2011;26(4):399-406.
16. Chua DT, Tian Y, Wei WI. Late oral complications following radiotherapy for head and neck cancers. Expert Rev Anticancer Ther. 2007;7(9):1215-1224.
17. Massey S. Esophageal cancer and palliation of dysphagia. Clin J Oncol Nurs. 2011;15(3):327-329.
18. Hasler WL. Nausea, vomiting, and indigestion. In: Kasper D, Fauci A, Hauser S, et al, eds. Harrison’s Principles of Internal Medicine. 19th ed. New York, NY: McGraw-Hill; 2014.
19. Clissold SP, Heel RC. Transdermal hyoscine (Scopolamine). A preliminary review of its pharmacodynamics properties and therapeutic efficacy. Drugs. 1985;29(3):189-207.
20. Basch E, Prestrud AA, Hesketh PJ, et al. Antiemetics: American Society of Clinical Oncology clinical practice guideline update [published correction appears in J Clin Oncol. 2014;32(19):2117]. J Clin Oncol. 2011;29(31):4189-4198.
21. Currow DC, Coughlan M, Fardell B, Cooney NJ. Use of odansetron in palliative medicine. J Pain Symptom Manage. 1997;13(5):302-307.
22. Ryan JL, Heckler CE, Roscoe JA, et al. Ginger (Zingiber officinale) reduces acute chemotherapy-induced nausea: a URCC CCOP study of 576 patients. Support Care Cancer. 2012;20(7):1479-1489.
23. Ezzo J, Vickers A, Richardson MA, et al. Accupuncture-point stimulation for chemotherapy-induced nausea and vomiting. J Clin Oncol. 2005;23(28):7188-7198.
24. Jobbins J, Bagg J, Finlay IG, et al. Oral and dental disease in terminally ill cancer patients. BMJ. 1992;304(6842):1612.
25. Löfgren CD, Wickström C, Sonesson M, et al. A systemic review of methods to diagnose oral dryness and salivary gland function. BMC Oral Health. 2012;12:29. http://www.biomedcentral.com/1472-6831/12/29. Accessed May 5, 2017.
26. Navazesh M, ADA Council on Scientific Affairs and Division of Science. How can oral health care providers determine if patients have dry mouth? J Am Dent Assoc. 2003;134(5):613-620.
27. Cooke C, Ahmedzai S, Mayberry J. Xerostomia—a review. Palliat Med. 1996;10(4):284-292.
28. Mandel ID. The role of saliva in maintaining oral hemostasis. J Am Dent Assoc. 1989;119(2):298-304.
29. Guggenheimer J, Moore PA. Xerostomia: etiology, recognition and treatment. J Am Dent Assoc. 2003;134(1):61-69.
30. DeWys WD, Walters K. Abnormalities of taste sensation in cancer patients. Cancer. 1975;36(5):1888-1896.
31. Smith G, Smith AJ, Shaw L, Shaw MJ. Artificial saliva substitutes and mineral dissolution. J Oral Rehabil. 2001;28(8):728-731.
32. Kielbassa AM, Shohadai SP, Schulte-Mönting J. Effect of saliva substitutes on mineral content of demineralized and sound dental enamel. Support Care Cancer. 2001;9(1):40-47.
33. Kleinegger CL. Dental management of xerostomia—opportunity, expertise, obligation. J Calif Dent Assoc. 2007;35(6):417-424.
34. Kerr AR, Corby PM, Shah SS, et al. Use of a mucoadhesive disk for relief of dry mouth: a randomized, double-masked, controlled crossover study. J Am Dent Assoc. 2010;141(10):1250-1256.
35. Turner M, Jahangiri L, Ship JA. Hyposalivation, xerostomia and the complete denture: a systemic review. J Am Dent Assoc. 2008;139(2):146-150.
36. Schelenz S, Abdallah S, Gray G, et al. Epidemiology of oral yeast colonization and infection in patients with hematological malignancies, head neck and solid tumors. J Oral Path Med. 2011;40(1):83-89.
37. Bagg J, Sweeney MP, Lewis MA, et al. High prevalence of non-albicans yeasts and detection of anti-fungal resistance in the oral flora of patients with advanced cancer. Palliat Med. 2003;17(6):477-481.
38. Budtz-Jørgenson E. Oral mucosa lesions associated with the wearing of removable dentures. J Oral Path. 1981;10(2):65-80.
39. Altieri KT, Sanitá PV, Machado AL, et al. Effectiveness of two disinfectant solutions and microwave irradiation in disinfecting complete dentures contaminated with methicillin-resistant Staphylococcus aureus. J Am Dent Assoc. 2012;143(3):270-277.
40. Sanita PV, Machado AL, Pavarina AC, et al. Microwave denture disinfection versus nystatin in treating patients with well-controlled type 2 diabetes and denture stomatitis: a randomized clinical trial. Int J Prosthodont. 2012;25(3):232-244.
41. Douglas WH, Walker DM. Nystatin in denture liners—an alternative treatment of denture stomatitis. Br Dent J. 1973;135(2):55-59.
42. Varhe A, Olkkola KT, Neuvonen PJ. Oral triazolam is potentially hazardous to patients receiving systemic antimyotics ketoconazole or itraconazole. Clin Pharmacol Ther. 1994;56(6 Pt 1):601-607.
43. Cobb MN, Desai J, Brown LS Jr, et al. The effect of fluconazole on the clinical pharmacokinetics of methadone. Clin Pharmacol Ther. 1998;63(6):655-662.
44. Massie MJ. Prevalence of depression in patients with cancer. J Natl Cancer Inst Monogr. 2004;32:57-71.
45. Wolff A, Zuk-Paz L, Kaplan I. Major salivary gland output differs between users and non-users of specific medication categories. Gerodontology. 2008;25(4):210-216.
46. de Gee AJ, van Duinen RN, Werner A, Davidson CL. Early and long-term wear of conventional and resin-modified glass ionomers. J Dent Res. 1996;75(8):1613-1619.
47. Donly KJ. Fluoride varnishes. J Calif Dent Assoc. 2003;31(3):217-219.
48. Heasman PA, Ritchie M, Asuni A, et al. Gingival recession and root caries in the ageing population: a critical evaluation of treatments. J Clin Periodontol. 2017;44(suppl 18):S178-S193.
49. Fusco F. Mouth care. In: Bruera E, Higginson IJ, Ripamonti C, von Ggunten C, eds. Textbook of Palliative Care. London, England: Hodder Arnold; 2006:773-779.
50. Fischer DJ, Epstein JB. Management of patients who have undergone head and neck cancer therapy. Dent Clin North Am. 2008;52(1):39-60.
51. Mirza N, Machtay M, Devine PA, et al. Gustatory impairment in patients undergoing head and neck irradiation. Laryngoscope. 2008;118(1):24-31.