You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.

The Static Impression Technique is used to create an accurate impression of undisturbed and uncompressed tissue.1,2 The Functional Impression Technique explains the need to make an impression based on the differing degrees of tissue function.3-5
Evaluation and Classification of Tissue Quality
After a thorough patient history has been obtained, the intraoral and extraoral structures should be evaluated closely. Inspecting intraoral tissue will permit the clinician to determine the character and mobility of the overlying soft tissue. Classifying the tissue after examination based on the differences between tissue character and mobility will give the clinician a simple method for selecting the appropriate viscosity to make the impression.
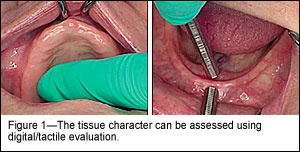
The clinician uses tactile manipulation to assess the character of the tissue overlying the bony support in the edentulous arches and classifies the tissue as either coarse and fibrotic, average, or thin and fragile. For example, if a patient's tissue quality is determined to be coarse and fibrotic covering the residual ridges, it is generally thought that the patient is able to tolerate a removable complete prosthesis better than if the supporting tissue is classified as thin and fragile.
The soft tissue overlying the residual ridges should be assessed using a blunt instrument to determine the relative amount of displacement or mobility. After tactile assessment, the tissue can then be classified and recorded as 1 of the following: attached, low mobility, low displacement; average, clinically acceptable displacement; or high mobility, high displacement. Soft tissue that is categorized as attached and less mobile overlying the alveolar ridge generally results in better adaptation of the removable prosthesis. Conversely, soft tissue quality that is categorized as high mobility and high displacement typically represents a clinical condition that is more difficult to manage and prepare for well-fitting complete dentures6 (Figure 1).
Materials
It has been demonstrated that the type of impression materials used for making the final impression can have a critical effect on the pressures produced during the impression making procedure; therefore, tray modifications have less significant influence when the amount of pressure produced needs to be controlled.7
In an attempt to select the most appropriate material for the technique, a review of the types of impression materials was completed. Materials considered included plaster, impression compound, zinc oxide eugenol, alginate, polysulfide, polyether, condensation silicone, and polyvinylsiloxane (addition-reaction silicone). Next, the important characteristics required to make a simultaneous static and functional impression were recorded8-10 (Table 1).
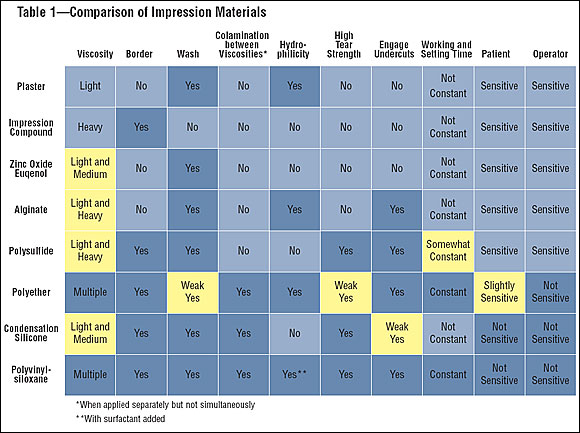
It is important to use an impression material that maintains dimensional stability during removal and re-insertion while making an impression that must be seated beyond anatomical undercuts.8 This requires a material with a high percentage of recovery from deformation.8 It is also important that the clinician be allowed to apply multiple viscosities sequentially and simultaneously that will set to form a homogeneous mass of impression material, regardless of the viscosity used. The materials selected for this technique must exhibit high tear strength (resistance to tearing) across the multiple viscosities used in this procedure.8,9 The use of the multiple viscosities of impression material should be such that there is a colamination between the layers of material and an anatomically correct and detailed reproduction that captures all aspects of the edentulous arches.
Based on the characteristics of the materials reviewed (Table 1), polyvinylsiloxane (PVS) materials appear to meet all of the requirements that support the use of this layering impression technique. The impression material used to demonstrate this technique is a hydrophilic, PVS material and a specially designed disposable edentulous tray. The authors chose Aquasil Ultra PVSa. Other PVS materials available are Clone Bite and Chromaclone PVS Super Lightb, Imprint 3c, and Extruded.
Clinical Application

For optimal intraoral access, appropriate lip and cheek retraction is made to assist the clinician during the impression-making procedures of the maxillary and mandibular arches (Figure 2). The high viscosity PVS impression material with low strain in compression is used initially to create tissue stops before proceeding (Figure 3). The low strain property of the material during compression helps reduce tissue movement or rebound after polymerization8 and helps to create predictable tissue stops when re-inserting the tray during subsequent steps. The tissue stops create adequate tissue relief for the impression material, help to reposition the impression intraorally, and center and stabilize the tray on the edentulous residual ridge. The tissue stops provide the clinician with a predictable position on tray re-insertion, helping to prevent over-seating the tray during functional border molding.

The impression tray is removed and excess impression material is trimmed. High viscosity PVS is then added to the borders of the maxillary impression tray, then border molded. The medium viscosity PVS is placed on the borders of the mandibular impression tray, then border molded. Each tray is border molded separately within the stated setting times (Figure 4). The high viscosity PVS used in this study captured anatomical details such as frena and the vestibular sulcus throughout and extended sufficiently to capture the postpalatal area in the border molding procedure for the maxillary arch. For the mandibular arch, it is important to preserve and maintain all frena, vestibular sulcus, retromylohyoid space, and the retromolar pads (Figure 5 and Figure 6).
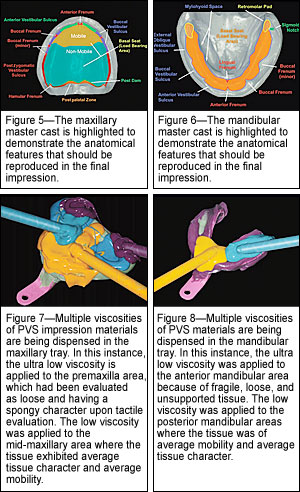
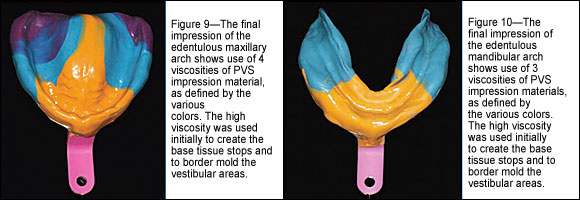
Dry the impression and place the appropriate viscosity impression material onto the basal seat (load-bearing area) as a thin "wash" impression; the appropriate viscosity of impression material selected is based on evaluation of the tissue character and mobility classification (Figure 7 and Figure 8). For example, the premaxilla and anterior mandibular areas displayed poor tissue character and mobility, which required the extra light viscosity material, while the posterior maxillary and mandibular arches displayed average tissue character and mobility, which suggested the need for low or average viscosity PVS material (Figure 9 and Figure 10). The clinician should inspect the accuracy of the impressions to ensure that all tissue details have been captured before pouring the master cast.
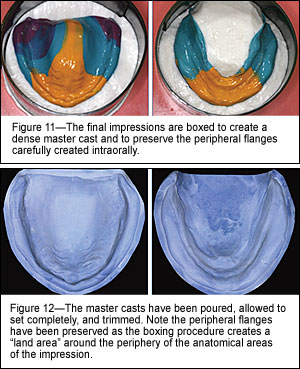
To preserve and protect the peripheral detail of the vestibular borders of the impressions, each final impression is boxed using the alginate boxing method. It is extremely important to maintain the peripheral borders of both the maxillary and mandibular impressions when boxing and to avoid over-trimming the master cast, which could compromise anatomical details of the vestibular borders (Figure 11). The selection and use of an appropriate dental stone is made in consideration of selecting one with controlled expansive/contractive properties9 (Figure 12).

Based on informal testing, it was found that the different viscosities applied and allowed to set simultaneously, could not be separated. However, the materials that were applied in separate layers (such as in a dual technique) exhibited more than adequate adhesion to each other and could only be separated with difficulty after several attempts. It should be noted that the adhesion between impression layers was enhanced when the layers were dried before placing the subsequent layer. Even in the presence of slight moisture contamination, the colamination between layers was sufficient to pour and create the master cast.
Conclusion
Making acceptable final impressions when fabricating complete dentures is an important requirement for the successful treatment of an edentulous patient. Diagnosing the tissue condition and classifying the edentulous arch11 should be the determining factors when selecting an impression technique for a specific patient. The layering technique presented in this article represents an alternate impression technique for the clinician who thoroughly understands the basic principles in complete prosthodontics and has the clinical ability to evaluate and assess intraoral tissues of the edentulous patient. The clinician can use multiple viscosities of an impression material and a stock edentulous tray (in this example, a well-designed disposable edentulous impression tray) to border mold and create an impression of the edentulous arch efficiently and accurately, as an effective clinical solution for the contemporary practice of treatment of the edentulous patient.
References
1. Bohannan HM. A critical analysis of the mucostatic principle. J Prosthet Dent. 1954;4:232-241.
2. Addison Pl. Mucostatic impressions. J Am Dent Assoc. 1944;31: 941-946.
3. Pendelton CE. The positive pressure technique of impression taking. Dent Cosmos. 1931;73:1045-1056.
4. Frank RP. Controlling pressures during complete denture impressions. Dent Clin North Am. 1970;14:453-470.
5. Boucher CO. A critical analysis of mid-century impression techniques for full dentures. J Prosthet Dent. 1951;1:472-491.
6. Massad JJ, Golijan KR. A method of prognosticating complete denture outcomes. Compend Contin Educ Dent. 1994;15:900-909.
7. Masri R, Driscoll CF, Burkhardt J, et al. Pressure generated on s simulated oral analog by impression materials in custom trays of different designs. J Prosthodont. 2002;11:155-160.
8. Anusavice, KJ. Phillips' Science of Dental Materials. 10th ed. Philadelphia, PA: Saunders; 1998.
9. Albers, HF. Impressions. A Texbook for Technique and Material Selection. 2nd ed. Santa Rosa,CA: Alto Books; 1990.
10. Ferracane, JL. Materials in Dentistry Principles and Applications. 2nd ed. Philadelphia, PA: Lippincott Williams and Wilkins; 2001.
11. McGarry TJ, Nimmo A, Skiba JF, et al. Classification system for complete edentulism. The American College of Prosthodontics. J Prosthodont. 1999;8:27-39.