You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
Today, life expectancy in the US has been estimated to have reached a record high of 77.8 years. The percentage of the population that is 75 years of age and older was 6% in 2005 and projected to double to 12% by 2050. While longer life expectancy is attributable to advances in healthcare, the prevalence of age-related chronic diseases and conditions will increase. From 2004 to 2005, the percentage of older adults with limited activity levels ranged from 25% among 65- to 74-year-olds to 60% of adults 85 years and older. Arthritis and other musculoskeletal conditions were the most common chronic medical morbidities that reduced activity in older individuals, followed by heart and circulatory problems. The percentage of adults with three or more ongoing conditions increased with age from 7% of those who are 45 to 54 years of age to 37% of people 75 years and older.1 Obviously, medication intake is higher with these chronic conditions, several of which are associated with dry mouth and related complications.2-5 This article will summarize the etiology, diagnosis, and management of xerostomia and salivary gland hypofunction, with emphasis on the elderly.
Definition
Xerostomia is a symptom defined as dry mouth, which may be associated with objective evidence of salivary gland hypofunction. A patient is considered to have reduced salivary flow if the unstimulated salivary flow is ≤ 0.1 mL/min measured for 5 to 15 minutes or if the chewing-stimulated salivary flow is ≤ 0.7 mL/min measured for 5 minutes.6-9
Prevalence
The prevalence of xerostomia in the general population is unclear because of the scant number of studies. Reports of the prevalence vary, ranging from 0.9% to 64.8%.10 The incidence of xerostomia increases from 6% at 50 years of age to 15% at 65 years of age.11 One finding estimated the occurrence of xerostomia in people 65 years and older to be approximately 30%.12 However, the prevalence reaches almost 100% in patients with Sjögren’s syndrome and those who are receiving radiation therapy for head and neck cancer.12
Etiology
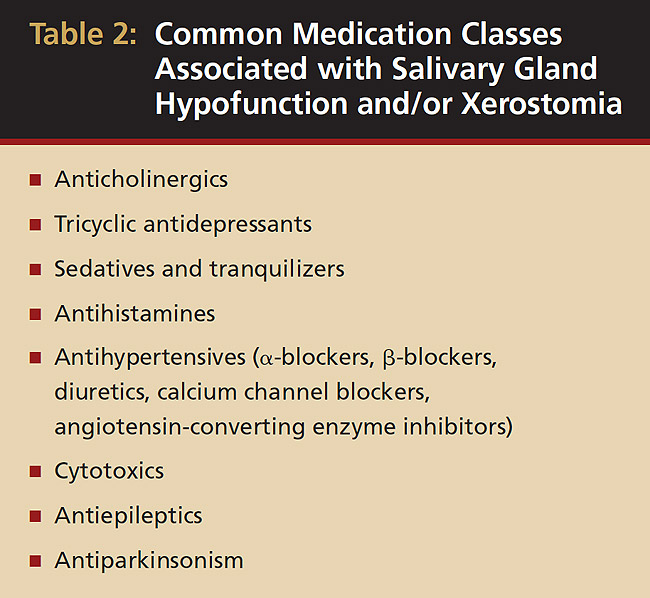
Aging per se has no significant impact on salivary gland secretion.12 In the elderly, several factors, such as decrease of ptyalin, increase of mucin, and low stimulation of the peripheral receptors, have been implicated in xerostomia.13 Xerostomia and/or salivary gland hypofunction in this population has been associated with a number of systemic disorders (Table 1) and medications14,15 (Table 2). The incidence increases with medication exposure,16 with more than 400 drugs implicated.2 In a 5-year longitudinal study, the relationship of dry mouth and long-term exposure to medications was assessed. Xerostomia severity was found to be higher among females and associated with the use of medications, such as antianginal, diuretics, antidepressants, and antiasthma, as well as thyroxine.17 Xerostomia and salivary gland hypofunction are also major complications of radiation or chemotherapy. Long-term morbidity in patients receiving combined radiation and chemotherapy is significant because of xerostomia, salivary gland hypofunction, and severe dysphagia.18

Clinical Presentation and Complications
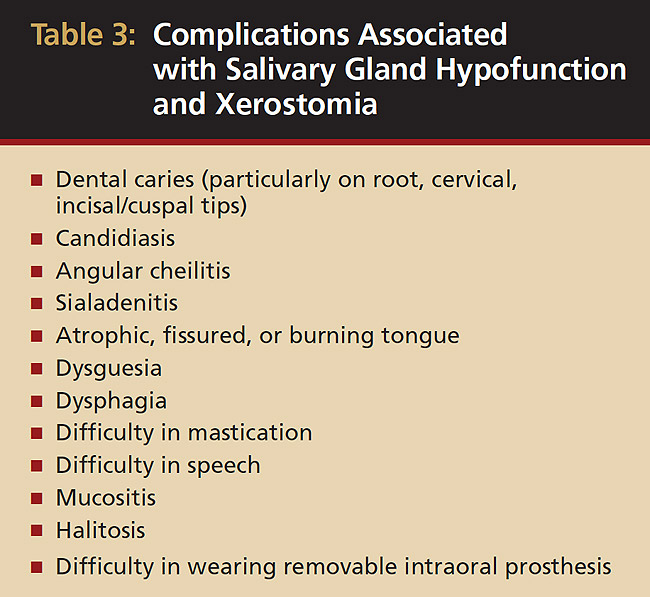
Saliva aids for oral cavity cleansing, swallowing, taste, speech, and digestion could be compromised in patients with salivary gland hypofunction. The oral mucosa may appear dry and friable. The tongue may appear dry and fissured (Figure 1). Dental caries, plaque accumulation, gingivitis, and periodontitis are common in patients with significant salivary gland hypofunction (Figure 2). Infections, such as oral candidiasis (Figure 3), and enlargement of salivary glands from sialadenitis are seen commonly in patients with moderate-to-severe salivary gland hypofunction (Figure 4). Difficulty in mastication and swallowing also may indicate advanced salivary gland hypofunction19 and can contribute to poor nutrition.20 Denture retention may become difficult because of the lack of saliva12 (Table 3).
Diagnosis
Oral healthcare providers can use a simple diagnostic algorithm to identify patients at risk of developing these problems21 and measure salivary flow rates for an objective assessment.22 Clinicians can use a simple questionnaire to assess dry mouth. A “yes” response to the following four questions has been associated with salivary gland hypofunction:9
- Does the amount of saliva in your mouth seem too little?
- Does your mouth feel dry when eating a meal?
- Do you have difficulty swallowing any food?
- Do you sip liquids to aid in swallowing dry food?
Visual analog scales and/or an ordinal scale based on ranked categories (eg, I have no/slight/severe/annoying feeling of dry mouth) also may be used.23 Objective measurements of both qualitative and quantitative changes in saliva are best performed by saliva collection from individual glands or all glands as reflected in whole saliva.22
A thorough medical history that includes the patient’s use of medications followed by clinical examination is necessary to establish a diagnosis. Further tests such as serologic evaluations (antinuclear antibodies, eg, rheumatoid factor, anti-Ro/anti-SS-A, anti-La/anti-SS-B), minor salivary gland biopsy (for detection of lymphocytic infiltration to eliminate systemic diseases, such as Sjögren’s syndrome or drug-induced sialadenitis), salivary gland imaging such as sialography and scintigraphy, and sialometric evaluations may be required to confirm the diagnosis and to determine any underlying systemic conditions. Consultation with physicians is critical to discuss if the medication responsible for xerostomia can be reduced in dosage or substituted with one that has little or no salivary side effects.
Management
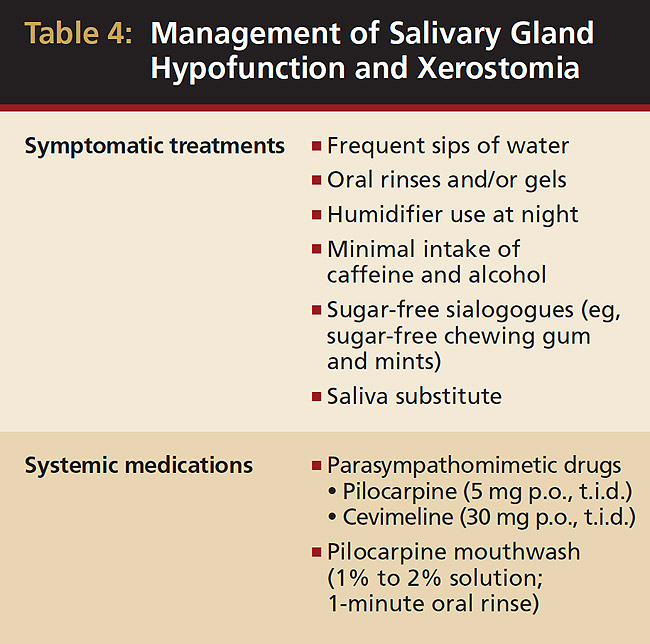
After determining a diagnosis and possible underlying causes, dental clinicians should begin management of these patients according to the severity of the condition. Symptomatic or palliative treatment of xerostomia, although transient, has proven to be beneficial and patient compliance is good (Table 4). Frequent sips of water as well as alcohol-free oral rinses, gels, mouthwashes, sugar-free chewing gum, and mints have all proven useful in reducing the feeling of dry mouth. Because xerostomia typically feels worse at night, use of a humidifier at night is helpful. Avoiding dehydration by minimizing caffeine and alcohol intake is recommended. Artificial saliva is typically not well-liked by patients and does not last.24 Severe salivary gland hypofunction and associated xerostomia can be managed by generalized parasympathomimetics, such as pilocarpine HCI (SALAGEN®, Pharmacia, Saint Paul, MN). However, the side effects of that medication, such as sweating, vasodilation, headaches, and urinary frequency, can decrease patient compliance.25 Cevimeline HCI (EVOXAC®, Daiichi Sankyo Inc., Tokyo, Japan) is another drug approved by the Food and Drug Administration (FDA) for treatment of oral dryness in Sjögren’s syndrome and administered as 30 mg, p.o., t.i.d.3,26 Pilocarpine HCI has been shown to be effective when used as a mouthwash for 1 minute in healthy individuals. This has shown to increase objective salivary flow (with 1% and 2% concentrations) and subjective salivary flow (with 2% concentration).27 Amifostine (Ethyol®, ALZA Corporation, Mountain View, CA) is effective in patients receiving radiotherapy.28 Amifostine is a thiol drug that is cytoprotective by several mechanisms, including scavenging oxygen-derived free radicals, deoxyribonucleic acid protection and repair acceleration, and induction of cellular hypoxia. The medication has FDA approval to reduce the incidence of moderate-to-severe xerostomia in patients undergoing postoperative radiation treatment for head and neck cancer.29-31
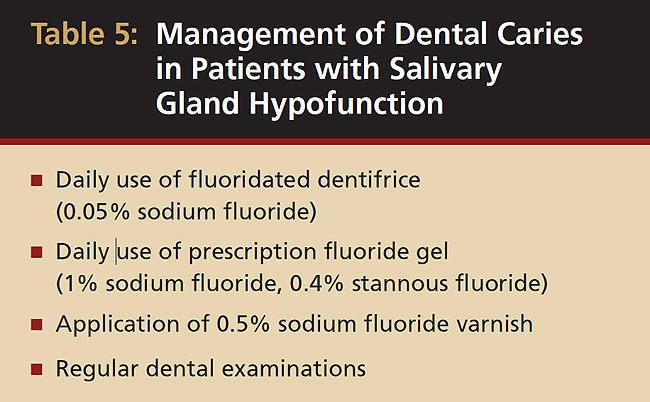
Fluorides, remineralizing solutions, and a noncariogenic diet are critical for preventing dental caries (Table 5). Regular dental examinations should be every 2 to 6 months, based on risk factors and disease susceptibility, such as past caries experience, periodontal status, quantity and quality of saliva, and disabling conditions that prevent oral hygiene maintenance.
Conclusion
The elderly population is expanding and so too are the rates of medical conditions and medication uses. This potentially may increase the prevalence of xerostomia and salivary gland hypofunction. Familiarity with contributing factors, clinical manifestations, and complications associated with xerostomia will help in better management. Preventive approaches will enhance quality of life in the elderly, who are more likely to have xerostomia.
References
1. Health, United States, 2007. Department of Health and Human Services, United States. http://www.cdc.gov/nchs/data/hus/hus07.pdf. Accessed February 10, 2009.
2. Sreebny LM, Schwartz SS. A reference guide to drugs and dry mouth—2nd edition. Gerodontology. 1997;14(1):33-47.
3. von Bültzingslöwen I, Sollecito TP, Fox PC, et al. Salivary dysfunction associated with systemic diseases: systematic review and clinical management recommendations. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103(suppl):S57.e1-e15.
4. Moore PA, Guggenheimer J. Medication-induced hyposalivation: etiology, diagnosis, and treatment. Compend Contin Educ Dent. 2008;29(1):50-55.
5. Mulligan R, Sobel S. Drugs commonly used by the elderly: a review for dental practice. J Calif Dent Assoc. 1994;22(3):35-47.
6. Navazesh M, Christensen C, Brightman V. Clinical criteria for the diagnosis of salivary gland hypofunction. J Dent Res. 1992;71(7): 1363-1369.
7. Ship JA, Fox PC, Baum BJ. How much saliva is enough? ‘Normal’ function defined. J Am Dent Assoc. 1991;122(3):63-69.
8. Tylenda CA, Ship JA, Fox PC, et al. Evaluation of submandibular salivary flow rate in different age groups. J Dent Res. 1988; 67(9):1225-1228.
9. Fox PC, Busch KA, Baum BJ. Subjective reports of xerostomia and objective measures of salivary gland performance. J Am Dent Assoc. 1987;115(4):581-584.
10. Orellana MF, Lagravère MO, Boychuk DG, et al. Prevalence of xerostomia in population-based samples: a systematic review. J Public Health Dent. 2006;66(2):152-158.
11. Johansson AK, Johansson A, Unell L, et al. A 15-yr longitudinal study of xerostomia in a Swedish population of 50-yr-old subjects. Eur J Oral Sci. 2009;117(1):13-19.
12. Ship JA, Pillemer SR, Baum BJ. Xerostomia and the geriatric patient. J Am Geriatr Soc. 2002;50(3):535-543.
13. Astor FC, Hanft KL, Ciocon JO. Xerostomia: a prevalent condition in the elderly. Ear Nose Throat J. 1999;78(7):476-479.
14. Navazesh M, Brightman VJ, Pogoda JM. Relationship of medical status, medications, and salivary flow rates in adults of different ages. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;81(2):172-176.
15. Wu AJ, Ship JA. A characterization of major salivary gland flow rates in the presence of medications and systemic diseases. Oral Surg Oral Med Oral Pathol. 1993;76(3):301-306.
16. Thomson WM, Chalmers JM, Spencer AJ, et al. A longitudinal study of medication exposure and xerostomia among older people. Gerodontology. 2006;23(4):205-213.
17. Thomson WM, Chalmers JM, Spencer AJ, et al. Medication and dry mouth: findings from a cohort study of older people. J Public Health Dent. 2000;60(1):12-20.
18. Nguyen NP, Sallah S, Karlsson U, et al. Combined chemotherapy and radiation therapy for head and neck malignancies: quality of life issues. Cancer. 2002;94(4):1131-1141.
19. Kaplan I, Zuk-Paz L, Wolff A. Association between salivary flow rates, oral symptoms, and oral mucosal status. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106(2):235-241.
20. Ritchie CS, Joshipura K, Hung HC, et al. Nutrition as a mediator in the relation between oral and systemic disease: associations between specific measures of adult oral health and nutrition outcomes. Crit Rev Oral Biol Med. 2002;13(3):291-300.
21. Navazesh M, Denny P, Sobel S. Saliva: a fountain of opportunity. J Calif Dent Assoc. 2002;30(10):783-788.
22. Navazesh M, Kumar SK; University of Southern California School of Dentistry. Measuring salivary flow: challenges and opportunities. J Am Dent Assoc. 2008;139(suppl):35S-40S.
23. Pai S, Ghezzi EM, Ship JA. Development of a Visual Analogue Scale questionnaire for subjective assessment of salivary dysfunction. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;91(3):311-316.
24. Turner MD, Ship JA. Dry mouth and its effects on the oral health of elderly people. J Am Dent Assoc. 2007;138(suppl):15S-20S.
25. Davies AN, Shorthose K. Parasympathomimetic drugs for the treatment of salivary gland dysfunction due to radiotherapy. Cochrane Database Syst Rev. 2007;(3):CD003782.
26. Petrone D, Condemi JJ, Fife R, et al. A double-blind, randomized, placebo-controlled study of cevimeline in Sjögren’s syndrome patients with xerostomia and keratoconjunctivitis sicca. Arthritis Rheum. 2002;46(3):748-754.
27. Bernardi R, Perin C, Becker FI, et al. Effect of pilocarpine mouthwash on salivary flow. Braz J Med Biol Res. 2002;35(1):105-110.
28. Sasse AD, Clark LG, Sasse EC, et al. Amifostine reduces side effects and improves complete response rate during radiotherapy: results of a meta-analysis. Int J Radiat Oncol Biol Phys. 2006;64(3):784-791.
29. Wasserman TH, Brizel DM, Henke M, et al. Influence of intravenous amifostine on xerostomia, tumor control, and survival after radiotherapy for head-and-neck cancer: 2-year follow-up of a prospective, randomized, phase III trial. Int J Radiat Oncol Biol Phys. 2005;63(4):985-990.
30. Sasse AD, Clark LG, Sasse EC, et al. Amifostine reduces side effects and improves complete response rate during radiotherapy: results of a meta-analysis. Int J Radiat Oncol Biol Phys. 2006;64(3):784-791.
About the Authors
Mahvash Navazesh, DMD, Professor and Chair, Division of Diagnostic Sciences; School of Dentistry, University of Southern California, Los Angeles, California
Satish K.S. Kumar, MDSc, Assistant Professor of Clinical Dentistry, Division of Diagnostic Sciences; School of Dentistry, University of Southern California, Los Angeles, California



