You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
The prevalence of periodontitis has been reported as 35% in the population of the United States1 and is likely underestimated.2,3 This percentage increases considerably with age.1 Restorative dentists and their staffs are usually a patient’s initial contact for addressing such oral health needs. This development in everyday oral healthcare practice is significant, as it places progressive demands on the periodontist to martial an increasingly complex skillset—particularly that of surgical implantology.
An increasingly educated patient population expects the replacement of individual missing or hopeless teeth with implants; typically, these requests are initially voiced to the restorative dentist. Such informed demand is keeping steadfast pace with the evolving comprehensive training and high levels of skill in implantology by periodontists.
Implantology is gradually but steadily acquiring a general-practice emphasis, and effective restorative-focused published resources4 and training programs5 are increasingly available. Studies by De Bruyn et al supported the capabilities of the restorative dentist to place restorations on implants placed by periodontists that achieve good clinical acceptability6 and patient satisfaction.7 And, while undergraduate dental curricula now impart the basics of success in surgical implantology,8-10 restorative dentists still rely on referrals to more surgically oriented practitioners such as periodontists and oral surgeons to place dental implants, especially if the surgical aspects are sophisticated. Hence, for effective multidisciplinary care, the need for quality communication channels and treatment-plan collaborations between periodontists and implant-focused restorative dentists has never been more critical.
The restorative-driven interdisciplinary approach was recently illustrated in a case report by Levine and Nack,11 which highlights the respective expertise of each practitioner—including the dental laboratory technician—for a surgical/restorative result that provided a high level of satisfaction for the patient. Vermylen et al12 noted patient ratings of acceptable to perfect quality of single-tooth implant-supported restorations placed by restorative dentists (with little or no experience placing implant restorations, but who had taken a postgraduate course) on fixtures placed by periodontists. The authors emphasize the importance of a team approach, as illustrated in the present article.
Esthetics are increasingly cited by a number of authors as a criterion for implant success.13,14 Zadeh reviewed the concept of implant site development in 2004, and even then cited the paradigm shift occurring in implantology whereby precise esthetic approximation of the natural dentition and periodontium is considered as important a criterion for implant success as osseointegration.15
Case 1
A 36-year-old nonsmoking Caucasian woman in good health presented to the author’s periodontal practice to replace tooth No. 26 with an implant. She had presented to her restorative dentist with a chief complaint of yellow, poorly color-matched mandibular anterior teeth (Figure 1). Her medical history was significant for asthma and seasonal allergies for which she took oral montelukast, orally inhaled fluticasone and salmeterol, and oral cetirizine; she also took lorazepam for anxiety. Her dental history was significant for traumatic experiences.
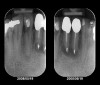
Radiographic evidence of external root resorption on tooth No. 26 and periapical radiolucencies with a history of prior endodontic treatment, including apicoectomies, were present on the mandibular central incisors (Figure 2).
Treatment Plan
The hopeless prognosis of tooth No. 26 and the questionable long-term prognoses of teeth Nos. 24 and 25, coupled with a desire to improve esthetics, motivated the patient to pursue treatment. Her objective was to replace these teeth with individual implants rather than a fixed bridge to facilitate ease of maintenance (flossing in particular).
Initially, only the nonrestorable tooth No. 26 was extracted by the periodontist, as the patient debated removing Nos. 24 and 25. The extraction site was filled with freeze-dried bone allograft (FDBA), and a porcine collagen membrane was secured with 4-0 chromic gut sutures.
A resin-based removable partial denture fabricated by the restorative dentist to replace No. 26 was delivered and adjusted by the periodontist. After further consultation, the patient approved removal of teeth Nos. 24 and 25 to reduce the risk of implant complications (ie, infection) from adjacent questionable endodontically treated teeth. However, based largely upon patient input, the somewhat unconventional decision was made to keep No. 23; because it was healthy, she wished to retain it and replace the remaining three incisors instead of replacing all four with two implants and a 4-unit bridge.
The periodontist and restorative dentist agreed, with the caveats that there would likely be a greater resulting gingival margin height on No. 23 relative to those of the adjacent implant crowns, and a flatter interproximal papillary architecture, which she accepted. She also found the resin partial denture increasingly difficult to tolerate and thus accepted the more comfortable and esthetic alternative proposed by the restorative dentist, ie, a fixed provisional covering the entire mandibular anterior segment. This also accommodated her esthetic needs and the planned full coverage on teeth Nos. 22, 23, 27, and 28.
The final treatment plan called for replacement of teeth Nos. 24 through 26 with implants, and four adjacent porcelain crowns. The restorative dentist prepared these four teeth for full coverage and decoronated Nos. 24 and 25, then, with patient input, selected a shade (Figure 3) and fabricated a bis-acryl temporary bridge from Nos. 22 to 28. After extracting teeth Nos. 24 and 25, the periodontist performed socket preservation in addition to horizontal ridge augmentation in site No. 26 with FDBA and a resorbable porcine collagen membrane. The flaps were approximated with 4-0 polyglactin 910 (Figure 4). Figure 5 shows the 7-unit bis-acryl temporary bridge.
Implant Placement
Six months later, the periodontist prepared osteotomies and placed three 3.25-mm x 13-mm implants using a vacuum-formed surgical guide fabricated by the restorative dentist (using a cast of the provisional bridge as a guide, as described by Block et al16); healing abutments were placed simultaneously. A post-implant radiograph confirmed good implant alignment with the pontics of the provisional from teeth Nos. 22 through 28 (Figure 6).
The implant placement procedure was performed under intravenous (IV) sedation to alleviate the patient’s dentally related anxiety. Following a 10-mg dose of oral midazolam, IV midazolam was titrated to achieve eyelid ptosis, and an infusion of 1 µg remifentanil per 1 mg propofol was given as a continuous infusion at a rate of approximately 25 µg/kg/min, in addition to oxygen via nasal-cannula (4 L/min). Standard American Society of Anesthesiology monitoring was maintained throughout the procedure, including capnography and use of a precordial stethoscope to continuously monitor airway patency. Anesthetic recovery was uneventful. Once adequate hemostasis was confirmed, ketoralac 30 mg and dexamethasone 6 mg IV were given postoperatively for pain and swelling, in addition to ondansetron 4 mg IV for postoperative nausea.
Restorative Phase
After the zirconia abutments were torqued to 20 Ncm, cotton and composite were used to cover the screw access openings. Figure 7 and Figure 8 show the finished feldspathic porcelain crowns on implants in sites Nos. 24 through 26, and on teeth Nos. 22, 23, 27, and 28; all crowns were cemented with dual-cure resin cement. Good remodeling of gingival architecture is also apparent in Figure 7. As predicted, the free gingival margin (FGM) on No. 23 is approximately 2 mm coronal to those of the adjacent implant crowns on Nos. 24 through 26 (Figure 7); as per the patient’s initial statement, this discrepancy was not an esthetic concern to her. Figure 9 shows the final post-restoration periapical view.
Case 2
Two years after sustaining a crown fracture, a 23-year-old healthy, nonsmoking Caucasian woman was referred to the author’s periodontal practice by her restorative dentist for replacement of her maxillary left central incisor with an implant. She was taking no medications and displayed a high smile line. Tooth No. 9 had been horizontally fractured when, as a passenger in a motorcycle accident, she was struck by her helmet, exposing the tooth’s vital pulp.
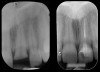
Emergency endodontic treatment had been completed to manage the traumatically exposed root canal; Figure 10 shows the pre-treatment (Ellis Class III crown fracture) and post–endodontic-treatment periapical views of tooth No. 9. The restorative dentist temporarily cemented a glass-reinforced fiber post and used a fiber-reinforced composite core buildup material as an immediate provisional. Several weeks later, a provisional bis-acryl temporary crown on No. 9 was cemented on a larger-diameter glass-reinforced fiber post retaining a new fiber-reinforced composite core. Figure 11 shows the final feldspathic porcelain crown placed by the restorative dentist. During the fabrication and cementation of this crown, the remaining root appeared intact and the tooth was asymptomatic.
Two years later, however, the patient returned to her restorative dentist’s office complaining that “something felt different” on tooth No. 9. Localized moderate gingival inflammation was present on the facial aspect of No. 9 (Figure 12). A straight facial probing depth of 6 mm and severe bleeding on probing were also evident facially, suggesting a vertical root fracture.
Treatment Plan
The collaborative treatment plan was to extract tooth No. 9, immediately replace it with an implant, and simultaneously provisionalize it with a temporary abutment and crown.
The restorative dentist designed a clear acrylic, vacuum-formed surgical guide. An access hole was placed through the cingulum area of the guide, because that was the intended screw access position for the final screw-retained restoration. The restorative dentist preferred a zirconia stock abutment, so care was taken to ensure precise alignment of the central implant axis with the surgical guide, to avoid the need for a custom abutment.
The periodontist carefully removed the existing crown and post with anterior forceps, then gently elevated the remaining root with a periotome. The extraction was performed atraumatically to preserve the facial cortical plate and existing gingival architecture, including the papilla and facial gingival margin; the socket then was thoroughly curetted, debrided, and irrigated.
A narrow 4-mm dehiscence defect was detected on the straight facial aspect of tooth No. 9. A flapless approach was maintained to preserve the blood supply to the remaining facial plate. Preservation of the hard- and soft-tissue volume around the implant impacts the final esthetics of the restoration.
The osteotomy was started slightly palatally in alignment with the surgical guide, using a 2.1-mm precision drill (Figure 13) and finalized with shaping drills under copious external irrigation with sterile water. Special attention was paid to overcorrecting the osteotomy preparation toward the palate, where the bone is denser. An implant in this area—especially a tapered implant, as was used here—will usually veer toward the facial surface during insertion. Using the surgical guide to superimpose the central axis of the implant on the previous location of the central incisor’s cingulum facilitates accurate positioning (Figure 14).
The periodontist positioned a 4.3-mm x 16-mm regular-platform implant flush with the facial crest and 1 mm subcrestally interproximally (Figure 15), with a manually driven final seating torque value > 50 Ncm, followed by hand-tightened attachment of the immediate temporary abutment.
Finally, particulate FDBA was placed into the implant-socket gap to help maintain the level of the facial gingiva, as was demonstrated in a case series by Tsuda et al.17 Facial plate augmentation was also performed to correct the narrow 4-mm dehiscence defect (Figure 16). Figure 17 shows the implant and abutment after graft placement. Human histologic evidence suggests that normal osseointegration and healing can occur without grafting or membranes, even with a substantial (≥ 4-mm) horizontal bony gap between the implant and facial wall in the esthetic zone.18 In this patient, a 2-mm horizontal gap and narrow 4-mm dehiscence were effectively managed with a particulate allograft, yielding a good esthetic result with immediate loading, owing in part to the minimally invasive technique utilized and the overall quantity and quality (Type 2) of bone involved.
Immediate loading and provisionalization with a temporary abutment were performed, as good initial stability was achieved (> 50 Ncm). In reporting retrospective data for up to 4 years post-immediate-loading of 94 implants in 49 patients (comprising 22 crowns in the maxillary esthetic zone, as with this patient), Malo et al set a minimum value of 32 Ncm as an inclusion criterion, achieving an overall 2-year success rate of 96%.19
Block et al16 proposed a 20-Ncm minimum torque value for immediate provisionalization in addition to other routine criteria such as sufficient bone height and mesiodistal and interocclusal clearances, with reported success rates of 94.6% (N = 74) for up to 2 years. In the author’s practice, the dental team immediately provisionalizes patients who display initial stability of ≥ 45 Ncm. Block et al16 prefer no occlusal contact; similarly, this patient’s restorative dentist placed this provisional crown out of protrusive occlusion.
Knowledge of inherent capabilities (and limitations) of guided bone regeneration (GBR) underscores the importance of case selection in determining functional loading protocols.
Restorative Phase
For the provisional implant crown, the restorative dentist relined a clear acrylic, vacuum-formed stent with bis-acryl and picked up the plastic sleeve packaged with the immediate temporary abutment. A convex subgingival profile was contoured to gently support the FGM circumferentially. The provisional crown was then cemented with non-eugenol-based temporary cement (Figure 18 and Figure 19).
The restorative dentist observed that the implant-retained temporary crown on No. 9 was slightly wider mesiodistally than No. 8 due to a slight midline discrepancy (Figure 19). Composite resin was added to the mesial aspect of No. 8, balancing the mesiodistal width, effecting a better tooth-size match, and providing cosmetic correction of the midline by moving it slightly to the left. The cement-retained bis-acryl provisional was maintained out of occlusion; this strategy was changed to light occlusion in protrusive for the final crown, and is in agreement with cautionary notes by Vermylen et al regarding porcelain stress arising from excessive occlusion (particularly in excursive movements) and compromised chewing with lack of occlusion.12
The restorative dentist preferred a screw-retained one-piece final restoration to facilitate retrievability, if ever necessary. The laboratory technician customized a zirconia stock abutment, applying multiple layers of a specialized porcelain whose coefficient of thermal expansion matched that of the zirconia abutment. A soft-tissue cast was created from the impression supplied by the restorative dentist. Additional layers of specialized zirconia porcelain were applied to develop the proper crown contour and emergence profile.
The final screw-retained crown was delivered and torqued onto the implant to 35 Ncm; the restorative dentist then sealed the screw access with a cotton pellet and composite (Figure 20 and Figure 21). Various views of the final crown are shown in Figure 22 through Figure 25, including a full-face photograph.
The patient, who works as a professional model, was pleased with her esthetic result, which was a paramount criterion for the team approach applied to this case, as emphasized by Vermylen et al, who reported positive to very positive ratings on esthetics and phonetics among 48 patients with 52 implants on which crowns were fabricated by their restorative dentists.12
Screw-Retained Vs. Cement-Retained Prostheses
While zirconia abutments show good clinical and biologic success in the short term,20 and zirconia crowns compare favorably with metal-ceramic implant-supported crowns at 1 year21—while demonstrating no complications when evaluated in a private practice setting over 5 years22—definitive clinical data are lacking to compare failure predisposition of screw- versus cement-retained zirconia implant crowns in the anterior maxilla. However, cautionary data suggest that some screw-retained implant crowns (posterior metal-ceramic) have lower fracture load values than cement-retained crowns.23 Another study suggested an overall poorer long-term prognosis (assessed at up to 180 months; 221 implants total), and significantly greater rates of ceramic fracture for screw-retained versus cemented implant crowns (P < 0.001).24 A systematic review by Weber and Sukotjo in 2007 did identify differences in success rates between cemented and screw-retained prostheses. They were, however, not statistically significant, and provided insufficient evidence to formulate a clinical guideline for selecting implant prosthesis type in the partially edentulous patient.25
Pre- and Postoperative Anti-microbial and Analgesic Protocol
Neither patient had any significant medical history to warrant preoperative antibiotic prophylaxis. However, both patients received preoperative antibiotic prophylaxis with 1 gram of amoxicillin administered orally 30 minutes prior to commencement of implant surgery.
Postoperatively, for all procedures, both patients received amoxicillin 875 mg twice daily for 7 days, ibuprofen 800 mg once every 6 hours, as needed for pain, and swabbing of the surgical area with chlorhexidine gluconate twice daily, beginning on the day after surgery. No postoperative infection occurred.
Assessment of Collaborative Clinical Outcomes
Case 1
Replacement of lower incisors in the esthetic zone can be one of the greatest challenges in restorative dentistry, especially in mimicking their morphology and gingival architecture. Of note, this perception parallels a relative lack of published clinical studies on mandibular-incisor replacement. Fleigel et al recently reviewed treatment options for replacing these teeth, citing anatomic, spatial, esthetic, and other challenges, and emphasizing the need for a multidisciplinary approach in managing such replacements.26
A recent retrospective analysis by Sohn et al27 reviewed the replacement of 54 mandibular and eight maxillary incisors (N = 36 patients; 62 implants total), with 1-piece 3-mm diameter implants, which were immediately provisionalized. They reported a 100% success rate at 33 months. Of note, most of these implants supported fixed bridges; only 18 were single-tooth replacements, as in the patient in Case 1. These results underscore the fact that even with a relatively large sample size, the number of single-tooth replacements addressed is small, as is the general trend in the literature.
Placement of any implant adjacent to periapical pathology requires definitive resolution in advance. Periapical lesions increasing in size to involve adjacent implants,28 and even osteomyelitis, which developed despite appropriate endodontic therapy on an implant-neighboring tooth, have been reported.29 In order to safeguard the planned adjacent implant sites, it was, therefore, necessary to extract teeth Nos. 24 and 25, whose endodontic prognoses were questionable, based on radiographic evidence.
Smith et al published a 10-case series on replacement of all four mandibular incisors, using two 3.25-mm diameter implants in the lateral-incisor positions, with the centrals replaced as pontics, showing a 100% survival rate over 6 years.30 In addition, a retrospective analysis of mandibular incisors replaced with narrow-neck implants by Cordaro et al identified a poorer prognosis when 2 adjacent mandibular incisors were replaced with individual implants, compared with single-tooth or multi-unit groups analyzed.31 The Case 1 patient’s hygienic demands precluded the multi-unit approach, as she insisted on three single-tooth replacements.
This patient faced a unique situation, perhaps not previously reported: retaining a healthy mandibular lateral incisor knowing this would create an esthetic compromise. Indeed, while the discrepancy in gingival-margin height is noticeable in retracted view (Figure 7), it does not show in full smile (Figure 8).
Case 2
The seemingly straightforward replacement of a single tooth can be more complicated than it appears at first observation, particularly in the anterior maxilla. Mirroring an adjacent central incisor—especially in a patient whose profession imposes stringent esthetic demands—required not only meticulous preservation of facial crestal and gingival architecture by the implant surgeon, but also the creation of a favorable subgingival profile in the final crown by the restorative dentist to support long-term soft-tissue esthetics. Again, this underscores the importance of a multidisciplinary approach.
A case report by den Hartog et al emphasizes a multidisciplinary maxillary anterior tooth replacement strategy. Similar to the current author’s approach, they used immediate loading, with contouring of the soft-tissue emergence profile for a screw-retained all-ceramic crown.32 In contrast, Minichetti and D’Amore used a staged approach with socket augmentation (bone allograft and a bovine collagen membrane) because of a missing facial wall on tooth No. 9.33
Buser et al reviewed the myriad unique challenges inherent in optimizing the esthetics of implant-supported restorations in the anterior maxilla. The authors highlighted proper implant positioning using a surgical guide, and the use of appropriate hard- and soft-tissue augmentation techniques, including GBR, ensuring facial-wall bony architecture conducive to an optimal esthetic result.34 This calls attention to the pivotal bearing of the periodontist’s skillset on preserving an ideal esthetic emergence profile for an implant-supported crown. Immediate single-tooth implant placement and provisionalization in the anterior maxilla were prospectively studied by Kan et al in 35 patients, noting a change of -0.55 mm +/- 0.53 mm in midfacial gingival height over 1 year; all were pleased with the esthetics and none noticed any change in this variable.35
The gingival frame of the final implant crown on tooth No. 9 successfully matched that of natural tooth No. 8 (Figure 23). Accomplishing this required not only preservation of the existing free-margin height, but also the mirroring of the zenith point (at the approximate junction of the middle and distal thirds of each incisor’s clinical crown).
Kinsel and Capoferri (restorative dentist and laboratory technician, respectively) emphasize maintaining the zenith with a harmonious FGM around implant crowns and adjacent teeth. They highlight the importance of provisional restoration contouring by the restorative dentist, and skillful modification of the master cast by the laboratory technician to emulate natural cementoenamel junction anatomy, whose convexity dictates the gingival frame.36 The provisional bis-acryl crown designed and fabricated by this patient’s restorative dentist enabled this elusive esthetic goal by introducing a slightly convex subgingival contour, establishing a lifelike emergence profile that was ultimately maintained in the definitive restoration (Figure 24).
Summary and Conclusion
Hard- and soft-tissue regeneration have become mainstream components of multidisciplinary restorative practice; restoration of the periodontium played integral roles in both cases discussed here and supports consistent conclusions from recent and long-standing data.
The repertoire of materials has expanded considerably, producing reports of reliable implant stability in regenerated sites prepared via approaches including: the use of nonexpanded polytetrafluoroethylene (PTFE) (420 cases)37; glycolide and trimethylene carbonate membrane placed over particulate autogenous bone with or without anorganic bovine bone-derived mineral (22 cases; mean 46 months follow-up)38; deproteinized bovine bone mineral (DBBM) versus bone-ceramic particulate (26 cases—decrease in buccolingual width was significantly greater with DBBM)39; lateral ridge augmentation using a mix of cancellous bone, freeze-dried allograft, and a biodegradable thermoplastic carrier, plus a resorbable membrane (73 private-practice cases)14; and recombinant bone morphogenetic protein-2.40
Restoration is a collective concept that speaks to function, esthetics, phonetics, and the overall health, benefit, mindset, and preferences of the patient. In this regard, the skillsets and philosophies of those who focus on restoring the periodontium and dentition (periodontist, restorative dentist, and dental laboratory technician) are inseparable.
Acknowledgments
The author thanks restorative dentists John Koutsoyiannis, DDS, and Andrew Reingold, DMD, of New York, New York for their collaborative patient care and restorative clinical photos of cases presented in this article; Adrian Jurim, MDT, Jurim Dental Studio, Inc., Great Neck, New York; Peter Kouvaris, CDT, Oral Design, Peter Kouvaris Dental Studio; Instructor, Full Mouth Reconstruction program, New York University College of Dentistry, New York, New York, for professional dental laboratory design and fabrication of the restorations in the cases; Louis Siegelman, DDS, Attending Dentist, Anesthesiologist, Lutheran Medical Center, Brooklyn, New York; Clinical Assistant Professor, New York University College of Dentistry; private practice, New York, New York, for administration of intravenous sedation for Case 1; and Scott A. Saunders, DDS, ELS, CMPP, of PragMed Manuscripts, Royersford, Pennsylvania, for professional medical writing and editing services in preparation of the manuscript.
References
1. Albandar JM, Brunelle JA, Kingman A. Destructive periodontal disease in adults 30 years of age and older in the United States, 1988-1994. J Periodontol. 1999;70(1):13-29.
2. Albandar JM. Underestimation of periodontitis in NHANES surveys. J Periodontol. 2011;82(3):337-341.
3. Eke PI, Thornton-Evans GO, Wei L, et al. Accuracy of NHANES periodontal examination protocols. J Dent Res. 2010;89(11):1208-1213.
4. Tischler M. Treatment planning implant dentistry: an overview for the general dentist. Gen Dent. 2010;58(5):368-374.
5. Hussaini S, Weiner S, Ahmad M. Implant survival rates in a condensed surgical and prosthetic training program for general practitioners in dental implants. Implant Dent. 2010;19(1):73-80.
6. De Bruyn H, Lindén U, Collaert B, Björn AL. Quality of fixed restorative treatment on Brånemark implants. A 3-year follow-up study in private dental practices. Clin Oral Implants Res. 2000;11(3):248-255.
7. De Bruyn H, Collaert B, Lindén U, et al. Patient’s opinion and treatment outcome of fixed rehabilitation on Brånemark implants. A 3-year follow-up study in private dental practices. Clin Oral Implants Res. 1997;8(4):265-271.
8. Bonde MJ, Stokholm R, Isidor F, Schou S. Outcome of implant-supported single-tooth replacements performed by dental students. A 10-year clinical and radiographic retrospective study. Eur J Oral Implantol. 2010;3(1):37-46.
9. Addy LD, Lynch CD, Locke M, et al. The teaching of implant dentistry in undergraduate dental schools in the United Kingdom and Ireland. Br Dent J. 2008;205(11):609-614.
10. Kido H, Yamamoto K, Kakura K, et al. Students’ opinion of a predoctoral implant training program. J Dent Educ. 2009;73(11):1279-1285.
11. Levine RA, Nack G. Team treatment planning for the replacement of esthetic zone teeth with dental implants. Compend Contin Educ Dent. 2011;32(4):44-50.
12. Vermylen K, Collaert B, Lindén U. Patient satisfaction and quality of single-tooth restorations. Clin Oral Implants Res. 2003;14(1):119-124.
13. Elian N, Ehrlich B, Jalbout Z, et al. A restoratively driven ridge categorization, as determined by incorporating ideal restorative positions on radiographic templates utilizing computed tomography scan analysis. Clin Implant Dent Relat Res. 2009;11(4):272-278.
14. Toscano N, Holtzclaw D, Mazor Z, et al. Horizontal ridge augmentation utilizing a composite graft of demineralized freeze-dried allograft, mineralized cortical cancellous chips, and a biologically degradable thermoplastic carrier combined with a resorbable membrane: a retrospective evaluation of 73 consecutively treated cases from private practices. J Oral Implantol. 2010;36(6):467-474.
15. Zadeh HH. Implant site development: clinical realities of today and the prospects of tissue engineering. J Calif Dent Assoc. 2004;32(12):1011-1020.
16. Block M, Finger I, Castellon P, et al. Single tooth immediate provisional restoration of dental implants: technique and early results. J Oral Maxillofac Surg. 2004;62(9):1131-1138.
17. Tsuda H, Rungcharassaeng K, Kan JY, et al. Peri-implant tissue response following connective tissue and bone grafting in conjunction with immediate single-tooth replacement in the esthetic zone: a case series. Int J Oral Maxillofac Implants. 2011;26(2):427-436.
18. Tarnow DP, Chu SJ. Human histologic verification of osseointegration of an immediate implant placed into a fresh extraction socket with excessive gap distance without primary flap closure, graft, or membrane: a case report. Int J Periodontics Restorative Dent. 2011;31(5):515-521.
19. Maló P, Rangert B, Dvärsäter L. Immediate function of Brånemark implants in the esthetic zone: a retrospective clinical study with 6 months to 4 years of follow-up. Clin Implant Dent Relat Res. 2000;2(3):138-146.
20. Ekfeldt A, Fürst B, Carlsson GE. Zirconia abutments for single-tooth implant restorations: a retrospective and clinical follow-up study. Clin Oral Implants Res. 2011;22(11):1308-1314.
21. Hosseini M, Worsaae N, Schiodt M, Gotfredsen. A 1-year randomised controlled trial comparing zirconia versus metal-ceramic implant supported single-tooth restorations. Eur J Oral Implantol. 2011;4(4):347-361.
22. Ortorp A, Kihl ML, Carlsson GE. A 5-year retrospective study of survival of zirconia single crowns fitted in a private clinical setting. J Dent. 2012;40(6):527-530.
23. Al-Omari WM, Shadid R, Abu-Naba’a L, El Masoud B. Porcelain fracture resistance of screw-retained, cement-retained, and screw-cement-retained implant-supported metal ceramic posterior crowns. J Prosthodont. 2010;19(4):263-273.
24. Nissan J, Narobai D, Gross O, et al. Long-term outcome of cemented versus screw-retained implant-supported partial restorations. Int J Oral Maxillofac Implants. 2011;26(5):1102-1107.
25. Weber HP, Sukotjo C. Does the type of implant prosthesis affect outcomes in the partially edentulous patient? Int J Oral Maxillofac Implants. 2007;22 suppl:140-172.
26. Fleigel JD III, Salmon CA, Piper JM II. Treatment options for the replacement of missing mandibular incisors. J Prosthodont. 2011;20(5):414-420.
27. Sohn DS, Bae MS, Heo JU, et al. Retrospective multicenter analysis of immediate provisionalization using one-piece narrow-diameter (3.0-mm) implants. Int J Oral Maxillofac Implants. 2011;26(1):163-168.
28. Shaffer MD, Juruaz DA, Haggerty PC. The effect of periradicular endodontic pathosis on the apical region of adjacent implants. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;86(5):578-581.
29. Sussman HI, Moss SS. Localized osteomyelitis secondary to endodontic-implant pathosis. A case report. J Periodontol. 1993;64(4):306-310.
30. Smith RB, Tarnow DP, Brown M, et al. Placement of immediate implants and a fixed provisional restoration to replace the four mandibular incisors. Compend Contin Educ Dent. 2009;30(7):408-415.
31. Cordaro L, Torsello F, Mirisola Di Torresanto V, Rossini C. Retrospective evaluation of mandibular incisor replacement with narrow neck implants. Clin Oral Implants Res. 2006;17(6):730-735.
32. den Hartog L, Raghoebar GM, Stellingsma K, Meijer HJ. Immediate loading and customized restoration of a single implant in the maxillary esthetic zone: a clinical report. J Prosthet Dent. 2009;102(4):211-215.
33. Minichetti JC, D’Amore JC. Socket repair utilizing collagen membrane and mineralized allograft in the esthetic zone: a case report. Gen Dent. 2010;58(5):410-415.
34. Buser D, Martin W, Belser UC. Optimizing esthetics for implant restorations in the anterior maxilla: anatomic and surgical considerations. Int J Oral Maxillofac Implants. 2004;19 suppl:43-61.
35. Kan JY, Rungcharassaeng K, Lozada J. Immediate placement and provisionalization of maxillary anterior single implants: 1-year prospective study. Int J Oral Maxillofac Implants. 2003;18(1):31-39.
36. Kinsel RP, Capoferri D. A simplified method to develop optimal gingival contours for the single implant-supported, metal-ceramic crown in the aesthetic zone. Pract Proced Aesthet Dent. 2008;20(4):231-236.
37. Barboza EP, Stutz B, Ferreira VF, Carvalho W. Guided bone regeneration using nonexpanded polytetrafluoroethylene membranes in preparation for dental implant placements—a report of 420 cases. Implant Dent. 2010;19(1):2-7.
38. Urban IA, Nagursky H, Lozada JL. Horizontal ridge augmentation with a resorbable membrane and particulated autogenous bone with or without anorganic bovine bone-derived mineral: a prospective case series in 22 patients. Int J Oral Maxillofac Implants. 2011;26(2):404-414.
39. Mardas N, Chadha V, Donos N. Alveolar ridge preservation with guided bone regeneration and a synthetic bone substitute or a bovine-derived xenograft: a randomized, controlled clinical trial. Clin Oral Implants Res. 2010;21(7):688-698.
40. Levin BP. Horizontal alveolar ridge augmentation: the importance of space maintenance. Compend Contin Educ Dent. 2011;32(8):12-21.
About the Author
Edward Gottesman, DDS
Clinical Assistant Professor
Department of Periodontics and Implant Dentistry
Stony Brook University School of Dental Medicine
State University of New York
Stony Brook
Private Practice
New York, New York