You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
Recently, several advancements in dental technology have been introduced that offer improved solutions to traditional endodontic problems. Advances in imaging, canal preparation, and the elimination of bacteria from the root canals have greatly improved endodontic procedures and their outcomes; examples of such technologies include hard tissue and soft tissue lasers, CAD/CAM systems, digital scanners, implant placement systems, and ultrasonic, laser-activated, and multi- sonic irrigation systems. At the same time, a paradigm shift has been occurring in the field of endodontics. According to a report of the American Association of Endodontists published in 2014, a staggering 70% of root canal treatments in the United States are completed by general dentists.1Considering that 15 million root canal treatments are performed annually in the United States,2it is evident that general dentists play a pivotal role in meeting a high demand for endodontic treatment, making it imperative that they be equipped with the necessary tools and knowledge to ensure successful outcomes for their patients.
This article describes the integration of advanced technology to achieve a single-visit workflow for root canal therapy that can be implemented by general practitioners. Driven by the need for efficient treatment and improved patient experience for patients who require root canal therapy, this new approach can help redefine the endo-restorative business model for general dentists. The aim of this article is to discuss the impact of various technological advances in irrigation on root canal therapy, the implementation of a one-day treatment workflow for root canal therapy followed by restorative treatment, and methods for treating complete root canal procedures with predictability.
CHALLENGES IN ENDODONTICS AND THE NEED FOR CHANGE
The introduction of gutta-percha as a root canal filling material and the development of rubber dam clamps once represented advancements in endodontics. The continued importance of these historical milestones is a testament to the longevity of certain materials and techniques in dentistry. Continuous improvement in endodontics remains as vital now as it was in the past. As Dr. W. Edward Deming explained, "It is not necessary to change. Survival is not mandatory."3
According to the American Association of Endodontists, the use of a rubber dam is the standard of care for any nonsurgical endodontic treatment, and as such, is considered integral to and essential for these procedures.4 This essential practice of tooth isolation is recommended to help prevent contamination, limit aerosols, protect tissues, and ensure overall patient safety. By contrast, there is limited guidance on techniques for performing other aspects of root canal treatment, specifically filing, shaping, irrigation, and restoration. The author has found that using large file sizes and filing the apex in the pursuit of perfect filing and shaping can result in unintended consequences such as perforations, removal of valuable tooth structure, and the susceptibility of teeth to fractures. Similarly, outdated approaches to cleaning the intricate root canal system has often led to unsatisfactory results.
With the introduction of micro-CT scanners, studies have shown the precise impact of various endodontic techniques on root canal anatomy, revealing that traditional endodontic techniques have never fully debrided parts of complex canals.5 The presence of bacteria after endodontic treatment, which may be promoted by delayed restorative treatment, remains a primary problem in patients who receive root canal therapy.6,7 Imaging also provides ample evidence of the prevalence of root canal complexities, such as cross canals, canals that do not extend beyond the middle of the tooth, and lateral canals. Because such canals are difficult to manipulate, file, and irrigate, complex root canal anatomy has historically been challenging to clean.
IRRIGATION TECHNOLOGIES
Root canal irrigants used in the chemical cleansing phase can be divided into two categories: antibacterial irrigants such as sodium hypochlorite (NaOCl) and chlorhexidine; and decalcifying irrigants such as citric acid and ethylenediaminetetraacetic acid (EDTA).8 NaOCl and EDTA are the most commonly used irrigants in endodontics owing to their complementary antimicrobial and decalcifying properties.8 Several technologies are available that can be used to activate NaOCl and enhance its effectiveness, such as syringe, ultrasonic, laser, and multisonic irrigation. Over the years, root canal irrigation technologies have evolved significantly to improve the effectiveness of disinfection within the root canal system. These advancements have yielded several advantages-as well as some disadvantages-that are worth exploring.
One common challenge of irrigation techniques is reaching all areas of the root canal system, such as intricate canal configurations, apical deltas, and lateral canals. Additionally, some irrigants may have limited antimicrobial properties or may be cytotoxic if used improperly, necessitating careful consideration of the irrigating solutions and their compatibility with the specific case.9
Syringe Irrigation
A widely used delivery method, syringe irrigation is one of the notable advancements in root canal irrigation. This technique involves the manual delivery of irrigation solutions into the root canal using a syringe and needle.10,11 Syringe irrigation provides the advantage of easy accessibility and simplicity, making it widely accessible and cost-effective. It allows for operator control of the flow and pressure of the irrigation solution, facilitating removal of debris and microorganisms from the canal. However, syringe irrigation has limitations, such as the inability to reach all areas of the root canal system and the potential for inconsistent irrigation due to variations in operator technique.11 To avoid the limitations of syringe irrigation, passive ultrasonic irrigation was introduced.
Passive Ultrasonic Irrigation
Ultrasonic irrigation of the root canal can be performed with or without simultaneous ultrasonic instrumentation. When canal shaping is not undertaken, the term passive ultrasonic irrigation (PUI) is used to describe the technique. Several systems are commercially available.
PUI involves the use of ultrasonic energy to activate and enhance the effectiveness of irrigating solutions. It has demonstrated enhanced cleaning over conventional methods, as PUI generates acoustic streaming and cavitation, which improves the penetration and diffusion of irrigants for cleaning and disinfection of the root canal system.12 PUI can reach and clean some areas of the root canal system that are difficult to access with conventional irrigation techniques.12
Disadvantages of PUI include the following:
• Learning curve. PUI requires proper training and mastery of technique to ensure its safe and effective use. Dentists need to familiarize themselves with the equipment, settings, and irrigation protocols to maximize the benefits of PUI and minimize the risk of complications.
• Equipment cost. The equipment required for PUI can be costly, which may pose a financial barrier for some dental practices. Equipment costs include the purchase of an ultra- sonic unit, handpieces, and compatible files or tips for activation.
Additional disadvantages as experienced by the author include:
• File deformation or separation. The ultrasonic energy used in PUI can cause deformation or separation of endodontic files. Excessive lateral pressure or improper technique can lead to file breakage, which may require additional steps for retrieval.
• Heat generation. PUI can generate heat due to the friction between the ultrasonic instrument and the irrigating solution. Excessive heat can cause damage to the periapical tissues, leading to postoperative complications.
• Limited access in curved canals. PUI may face limitations in severely curved canals or areas with complex anatomy. The efficiency of ultrasonic activation decreases as the curvature increases, making it challenging for PUI to reach all areas of the root canal system.
It is important to note that these advantages and disadvantages vary. The effectiveness and challenges associated with PUI likewise may vary depending on the specific case, operator proficiency, and equipment used.13
Laser-Activated Irrigation
More recently, laser-activated irrigation (LAI) has emerged as a promising technology for root canal disinfection. LAI involves the use of laser energy to activate irrigating solutions within the root canal, enhancing their antimicrobial efficacy. A recent literature review concluded that irrigation with laser activation has superior efficacy over irrigation with ultrasonic activation.14 Photo- activation techniques with cavitation led to better results than ultrasonic methods, when used for the same amount of time, with greater removal of debris. However, because light travels in only one direction and, in the absence of thousands of mirrors, a laser can heat only the fluid in the canal at which it is directed, LAI cannot effectively reach anatomy that it cannot "see" directly.15
Disadvantages of LAI include:
• Equipment cost. The initial capital expenditure and subsequent operating costs for various components can be a disadvantage.8
• Case limitations.Laser light is emitted in a straight line, which can make it difficult to achieve uniform irradiation of the entire root canal dentin surface. Additionally, laser and retreatment procedures in curved root canals can be dangerous due to the risk of creating ledges and perforations.16
• Risk of thermal damage.There is a risk of thermal damage to the surrounding tissues.16
Multisonic Irrigation
One solution that has been introduced to address the challenges presented by complex canal anatomy and the persistence of bacteria after endodontic procedures is multisonic irrigation. The multisonic irrigation system standardizes root canal treatment with an automated protocol that administers an 8-minute sequence of NaOCl, distilled water, and EDTA,17 refreshing the irrigants 50 to 60 times throughout the treatment process. Simultaneously, expended irrigants and debris are cycled out of the system. To achieve optimized fluid distribution throughout the root canal system, as well as prevent vapor lock, a phenomenon that occurs in almost all endodontic treatments otherwise,18each irrigant is degassed before treatment begins.19As irrigants are cycled into the tooth, a continuous cavitation cloud of tiny imploding vapor bubbles is created by the irrigation system.17These implosions create a constant barrage of shockwave energy-ie, multisonic energy-that vibrates within the irrigants as they travel through the canals and disrupts and dissolves the pulp, biofilm, and other debris within the canals19-21; in some recent manufacturer-supported studies, multisonic irrigation was found to be significantly more effective at tissue dissolution22and demonstrated a greater cleaning capacity and reduction of residual debris within the mesiobuccal and mesiolingual canals of mandibular molars23 than the conventional irrigation methods evaluated in these studies. The degassing of the irrigants helps prevent the damping of the acoustic energy as it moves through the canal anatomy.20 Finally, according to some manufacturer- sponsored studies, as the irrigant stream passes throughout the canals, vortical flow is created, producing negative pressure that guards against apical extrusion.24-27 Multisonic irrigation has also been found to cause minimal dentin erosion.28
In the author's experience, a multisonic irrigation system is useful for premolars, first and second molars, and anterior teeth that require root canal therapy. Multisonic irrigation is well-suited for teeth with complex root canal anatomy.17 Contraindications include: third molars, primary dentition, teeth with open apices, molar teeth without a pulpal floor, teeth with fractured roots or unrestorable root perforations, subgingival decay, and/or resorption, maxillary teeth with direct communication with the maxillary sinus cavity, and any procedural error (eg, filing past the apex) that results in the penetration or breakage of the maxillary sinus floor, and it should not be used in patients with an implantable medical device (eg, pacemaker, defibrillator) or in patients with a known sensitivity to polycarbonate, silicone, NaOCl, or EDTA.29
Disadvantages of multisonic irrigation include:
• Learning curve.As with PUI, multisonic irrigation re- quires proper training to learn the proper operation of equipment, procedure preparation, and irrigation protocols.
• Equipment cost. The initial capital expenditure and sub- sequent operating costs for consumables, primarily in single- use handpieces, are high.
ACHIEVING SINGLE-VISIT ENDO-RESTORATIVE TREATMENT
Delayed restoration following root canal therapy can promote the risk of bacterial invasion. To overcome this challenge, the author has implemented a one-day treatment workflow for root canals. This workflow involves the traditional steps followed in root canal procedures of administering anesthetics, isolating the tooth with a dental dam, accessing the tooth, locating the canals, determining the working length, performing minimal instrumentation, building platforms, irrigating the canals, drying and obturating, and placing a crown; however, with this workflow, these steps are accomplished all within a single visit. By streamlining the process and leveraging advanced technology, the endo- restorative business model can be redefined for general dentists, while elevating the standard of care that is provided to endodontic patients.
The implementation of a one-day treatment workflow requires careful planning, preparation, and collaboration among the dental team. It is crucial to have a dedicated assistant who is well-versed in the steps involved and capable of managing the various components seamlessly. Additionally, it is essential to educate patients about the benefits and efficiency of the one-day approach, ensuring that they have realistic expectations and are comfortable with the treatment plan.
The first step in the one-day treatment workflow consists of meticulous diagnosis and treatment planning. This involves conducting a comprehensive examination, including radiography and other imaging modalities to evaluate the tooth's condition. Careful consideration is given to factors such as the presence of periapical pathology, root morphology, and the overall prognosis of the tooth. Based on this evaluation, a decision is made regarding the feasibility of a one-day treatment approach.
The next step is administration of anesthesia. Local anesthesia is administered to ensure the patient is comfortable throughout the procedure. Effective isolation is crucial to maintaining a clean and dry operative field, preventing contamination, and improving treatment predictability. The traditional rubber dam technique is employed for isolation, as it remains the gold standard in achieving optimal results.
After anesthesia has been administered to the patient and isolation is in place, the practitioner then proceeds to gain access to the root canal system. This step involves carefully removing the existing restorations and creating a small access opening through which the pulp chamber can be reached. It is essential to maintain a conservative approach while accessing the pulp chamber to preserve the tooth's structural integrity.
Once access is achieved, the next crucial step is determining the working length and establishing the glide path. This is accomplished using an apex locator and a small, flexible hand file. By accurately determining the working length, the practitioner ensures that the subsequent steps of cleaning and shaping the root canal system are performed effectively and with precision.
The cleaning and shaping of the root canal system are vital to eliminate bacteria, infected tissue, and debris. In the one-day treatment workflow, multisonic irrigation technology is employed to enhance the cleaning process of the root canal system. This irrigation system utilizes multisonic energy, as described earlier, to effectively eliminate microorganisms such as multispecies biofilms that are often resistant to traditional irrigation solutions13 and delivers fluid throughout the entire root canal system.15,17,19
The next phase involves obturation-the process of filling the root canal space. The author recommends employing a warm vertical obturation technique using a bioceramic sealer and a gutta- percha cone. This combination provides excellent sealability and biocompatibility, facilitating the long-term success of the root canal treatment.
Once the root canal is filled, the focus shifts to creating post space and performing a build-up. These steps are crucial for providing structural support to the tooth and preparing it for the final restoration. Utilizing a fiber post and a dual-cured core build-up material ensures the stability and longevity of the tooth.
The final step in the one-day treatment workflow is the placement of a crown. After the post and core build-up have been completed, the tooth is prepared for a definitive restoration. Utilizing CAD/CAM technology, the practitioner should capture digital impressions of the tooth; this eliminates the need for traditional impressions. The digital impressions are then transferred to a chairside milling unit, which fabricates a custom crown with exceptional accuracy and efficiency. The crown is then bonded to the tooth using adhesive techniques, providing a natural-looking and durable restoration.
This one-day treatment workflow has the potential to redefine the endo-restorative business model, and as such, it marks a significant achievement for endodontics. By integrating advanced technology, streamlining procedures, and leveraging the expertise of the dental team, we can improve the patient experience and elevate the standard of care. The one-day approach offers numerous benefits, including reduced treatment time, enhanced patient comfort, and improved treatment outcomes. Moreover, it empowers general dental practitioners to confidently undertake root canal procedures, effectively bridging the gap between demand and specialized care.
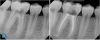
Figure 1 and Figure 2 provide examples of some cases that the author treated using the single-visit endo-restorative workflow. Despite the complex or challenging anatomy shown in these radiographs, the canals were able to be thoroughly irrigated by the multisonic irrigation system that was used with this workflow. For these cases, the one-day treatment workflow and the use of multisonic irrigation as described in this article enabled successful root canal treatment and improved patient satisfaction.
CONCLUSION
The integration of advanced irrigation technology can enable a single-visit workflow for endodontics and level-up the way that root canal procedures are performed, making it possible for general dental practitioners to undertake root canal treatment and restorative treatment on the same day and thereby prevent bacterial invasion in the restored tooth. By leveraging technologies such as multisonic irrigation for their patients who require root canal therapy, general dentists can enhance the patient experience, improve treatment efficiency, and achieve predictable outcomes.
References
1. Savani GM, Sabbah W, Sedgley CM, Whitten B. Current trends in endodontic treatment by general dental practitioners: report of a United States national survey. J Endod. 2014;40(5):618-624.
2. Niazi SA, Bakhsh A. Association between endodontic infection, its treatment and systemic health: a narrative review. Medicina (Kaunas). 2022;58(7):931.
3. Scherkenbach WW. Demin's Road to Continual Improvement.Knoxville, TN: SPC Press;1991:57-90.
4. American Association of Endodontists Clinical Practice Committee. Dental Dam. AAE Position Statement. Available at: https://www.aae.org/specialty/wp-content/uploads/sites/2/2017/06/dentaldamstatement.pdf. Published 2017. Accessed July 20, 2023.
5. Karobari MI, Arshad S, Noorani TY, et al. Root and root canal configuration characterization using microcomputed tomography: a systematic review. J Clin Med.2022;11(9):2287.
6. Prada I, Micó-Muñoz P, Giner-Lluesma T, Micó-Martínez P, Collado-Castellano N, Manzano-Saiz A. Influence of microbiology on endodontic failure. Literature review. Med Oral Patol Oral Cir Bucal.2019;24(3):e364-e372.
7. Endo MS, Ferraz CC, Zaia AA, Almeida JF, Gomes BP. Quantitative and qualitative analysis of microorganisms in root-filled teeth with persistent infection: monitoring of the endodontic retreatment. Eur J Dent.2013;7(3):302-303.
8. Dioguardi M, Di Gioia G, Illuzzi G, Laneve E, Cocco A, Troiano G. Endodontic irrigants: different methods to improve efficacy and related problems. Eur J Dent.2018;12(3):459-466.
9. Ghivari SB, Bhattacharya H, Bhat KG, Pujar MA. Antimicrobial activity of root canal irrigants against biofilm forming pathogens - an in vitro study. J Conserv Dent.2017;20(3):147-151.
10. Tashkandi N, Alhamdi F. Effect of chemical debridement and irrigant activation on endodontic treatment outcomes: an updated overview. Cureus. 2022;14(1):e21525.
11. Teja KV, Ramesh S, Battineni G, Vasundhara KA, Jose J, Janani K. The effect of various in-vitro and ex-vivo parameters on irrigant flow and apical pressure using manual syringe needle irrigation: systematic review. Saudi Dent J. 2022;34(2):87-99.
12. Plotino G, Grande NM, Mercade M, et al. Efficacy of sonic and ultrasonic irrigation devices in the removal of debris from canal irregularities in artificial root canals. J Appl Oral Sci.2019;27: e20180045.
13. Paixão S, Rodrigues C, Grenho L, Fernandes MH. Efficacy of sonic and ultrasonic activation during endodontic treatment: a meta-analysis of in vitro studies. Acta Odontol Scand.2022;80(8):588-595.
14. Badami V, Akarapu S, Kethineni H, Mittapalli SP, Bala KR, Fatima SF. Efficacy of laser-activated irrigation versus ultrasonic- activated irrigation: a systematic review. Cureus.2023;15(3): e36352.
15. Anagnostaki E, Mylona V, Parker S, Lynch E, Grootveld M. Systematic review on the role of lasers in endodontic therapy: valuable adjunct treatment? Dent J (Basel). 2020;8(3):63.
16. Jurič IB, Anić I. The use of lasers in disinfection and cleanliness of root canals: a review. Acta Stomatol Croat. 2014;48(1):6-15.
17. Choi HW, Park SY, Kang MK, Shon WJ. Comparative analysis of biofilm removal efficacy by multisonic ultracleaning system and passive ultrasonic activation. Materials (Basel).2019;12(21):3492.
18. Puleio F, Lizio AS, Coppini V, Lo Giudice R, Giudice GL. CBCT-based assessment of vapor lock effects on endodontic disinfection. Appl Sci. 2023;13(17):9542.
19. Jaramillo DE, Arriola AR. Histological evaluation of multi- sonic technology for debridement of vital and necrotic pulp tissues from human molar teeth. an observational study. Appl Sci.2021;11(22):11002.
20. Liu H, Shen Y, Wang Z, Haapasalo M. The ability of different irrigation methods to remove mixtures of calcium hydroxide and barium sulphate from isthmuses in 3D-printed transparent root canal models. Odontology.2022;110(1):27-34.
21. Sharma N, Alobaid MA, Nayan K, et al. Effectiveness of removal of hard tissue debris from the mesial root canal system of mandibular molars using different supplementary irrigation protocols: an original study. J Pharm Bioallied Sci. 2023;15(Suppl 1):S151-S155.
22. Liu H, Shen Y, Haapasalo M. Effectiveness of six irrigation techniques with sodium hypochlorite in tissue dissolution. Cureus. 2023;15(5):e39208.
23. Molina B, Glickman G, Vandrangi P, Khakpour M. Evaluation of root canal debridement of human molars using the GentleWave system. J Endod. 2015;41(10):1701-1705.
24. Chen B, Shen Y, Ma J, Haapasalo M. Effect of apical size on apical pressure during syringe-needle and multisonic negative pressure irrigation. Odontology. 2021;109(3):625-631.
25. Haapasalo M, Shen Y, Wang Z, et al. Apical pressure created during irrigation with the GentleWave™ system compared to conventional syringe irrigation. Clin Oral Investig. 2016;20(7): 1525-1534.
26. Ordinola-Zapata R, Crepps JT, Arias A, Lin F. In vitro apical pressure created by 2 irrigation needles and a multisonic system in mandibular molars. Restor Dent Endod. 2021;46(1):e14.
27. Charara K, Friedman S, Sherman A, et al. Assessment of apical extrusion during root canal irrigation with the novel GentleWave system in a simulated apical environment. J Endod. 2016;42(1): 135-139.
28. Wang Z, Maezono H, Shen Y, Haapasalo M. Evaluation of root canal dentin erosion after different irrigation methods using energy- dispersive x-ray spectroscopy. J Endod. 2016;42(12):1834-1839.
29. GentleWave® System [Instructions for Use]. Laguna Hills, CA: Sonendo, Inc.; revised August 2023.